Tashia Dare
Introduction
When studying the history of medicine, names such as the Greek physicians Hippocrates (circa 460–circa 375 BCE) and Galen (129 CE–circa 216 CE) immediately come to mind. Modern medicine is indebted to the ancient Greeks, but it is equally important to study the development of medicine in the ancient Near East before the Hellenistic period. As this section will demonstrate, we are just as indebted to the ancient Egyptians as we are to the Greeks.
Medicine in ancient Egypt incorporated both conventional (rational) medicine and religious practices. Religion played a major role in ancient Egyptian daily life. There was an overlap between the priesthood and healers in addition to the frequent employment of incantations, amulets, and imagery related to deities such as Horus and Seth.[1] The Egyptians’ religious life and views helped shape their understanding of the human body, how it functions, and how to heal it.
Ancient Egyptians recognized health and illness as expressions of an individual’s relationship with the world, which comprised people, animals, spirits, and gods.[2] Although they saw a distinction between the mundane/mortal and the supernatural/divine, they saw these worlds as frequently interacting with one another. Maat (order, balance, justice) was an integral part of this, governing people’s actions and approaches to healing illnesses and injuries (fig. 1).
 Figure 1. Scarab inscribed for Maatkare (Hatshepsut), New Kingdom, Eighteenth Dynasty (1479–1458 BCE). In the center of the base of the scarab in the cartouche is Hatshepsut’s throne name, Maatkare (Hatshepsut was queen and later pharaoh during the Eighteenth Dynasty). Maatkare generally translates as “Maat is the life force of Re (the sun god).” On either side of the cartouche are feathers representing the goddess Maat (truth). Above the cartouche is a winged sun disk and below is a broad collar with falcon terminals. Steatite (glazed), 1.8 × 1.3 cm (11/16 × 1/2 in.). New York Metropolitan Art Museum, Rogers Fund, 1927, 27.3.230.
Figure 1. Scarab inscribed for Maatkare (Hatshepsut), New Kingdom, Eighteenth Dynasty (1479–1458 BCE). In the center of the base of the scarab in the cartouche is Hatshepsut’s throne name, Maatkare (Hatshepsut was queen and later pharaoh during the Eighteenth Dynasty). Maatkare generally translates as “Maat is the life force of Re (the sun god).” On either side of the cartouche are feathers representing the goddess Maat (truth). Above the cartouche is a winged sun disk and below is a broad collar with falcon terminals. Steatite (glazed), 1.8 × 1.3 cm (11/16 × 1/2 in.). New York Metropolitan Art Museum, Rogers Fund, 1927, 27.3.230.One’s good health meant that maat was balanced, while illness, injuries, and other issues indicated that maat was not in order. Health depended on this balance just like Egypt depended on the Nile River to maintain life.[3] Purity preserved maat and thus the body guided views on the relationship between the mortal world and the divine. Being pure was particularly important when one was coming into contact with the divine, including priests. To not be so could anger the gods.[4] The swnw (conventionally pronounced as “sewnew”), wab priest, and sau were healers who focused either on the divine or mortal aspects of an illness or injury.[5] They turned to the religious idea that illness was a message from divine entities with access to heka (magic power). Symptoms were a result of a disturbance of maat, which could be repaired by heka, supplication, spells, and ritual.[6]
Much of what we know about ancient Egyptian medicine comes from human remains, visual representation as seen in tombs and temples, among other places, and through written texts. The beginning of organized medical care and the development of Egyptian medical science may be credited to Imhotep, during the reign of Pharaoh Djoser of the Third Dynasty (circa 2686–2613, Old Kingdom). Clemens of Alexandria (150–215 CE) noted that this knowledge may have existed much earlier with Athothis of the First Dynasty (circa 3100–2890); (son of Menes, the first pharaoh and who united Upper and Lower Egypt) and who may have authored a volume on anatomy.[7]
The Corpus of Medical Papyri
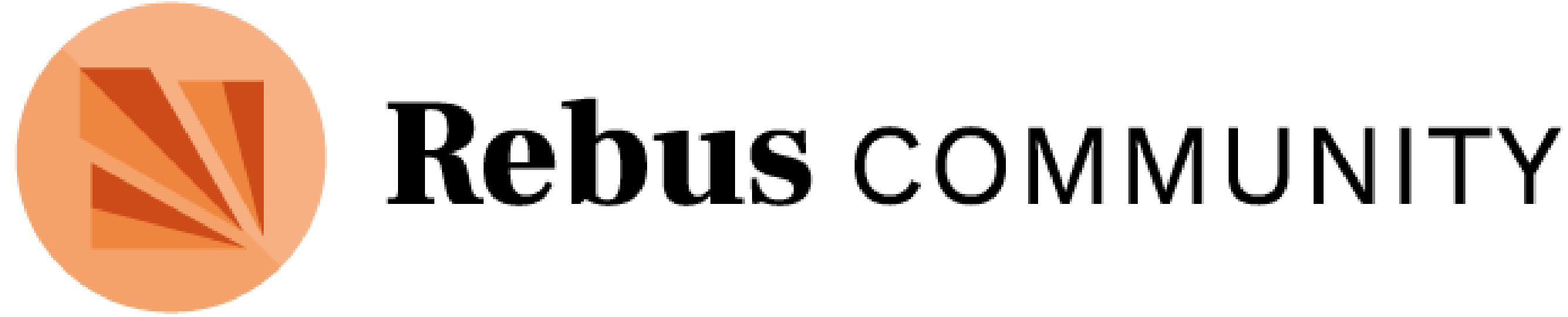
Much of what we know about ancient Egyptian medicine has been preserved through several medical papyri. Many of the surviving papyri have been found in tombs. Before the discovery of these papyri, much of what we knew was through the writings of individuals like Hippocrates, Homer, Herodotus, Pliny the Elder, and Diodorus.[8] Although the papyri are in various states of preservation, they give us valuable insight into the ancient Egyptians’ knowledge of human anatomy and physiology, ways of diagnosing disease and injuries, and how to treat medical issues using both rational medicine and magico-religious (a belief in supernatural beings) elements. Presently, there are at least eleven known medical texts (in chronological order): the Kahun, Ramesseum, Edwin Smith, Ebers, Berlin, Hearst, London, Chester Beatty, Carlsberg, Brooklyn, and the London-Leiden Papyrus (fig. 2).[9]
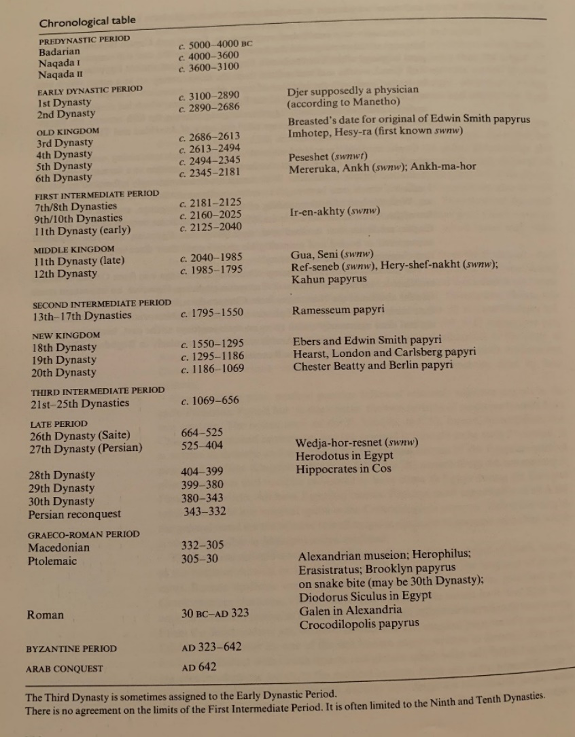
Figure 2. List of significant ancient Egyptian medical papyri. From John F. Nunn, Ancient Egyptian Medicine (Norman: University of Oklahoma Press, 1996).
All of these papyri were composed in hieratic except Ramesseum V, which is in cursive hieroglyphs, much like the Kahun veterinary text. Later papyri were composed mainly in demotic, which was the dominant script.[10] Hieratic and cursive hieroglyphs were used at the same time and within a medical setting. Thus, they may have been understood by most physicians. Hieratic is a cursive form of Egyptian hieroglyphs that could be written quickly on papyri for administrative and literary purposes, while cursive hieroglyphs were used mainly in religious texts (including the Book of the Dead). Demotic was primarily used for administrative purposes but over time also came to be used for literary, science, and religious documents.[11] There is no clear reason why the Ramesseum V and the Kahun texts were written in a different script than the other texts. There is reason to believe that we only have a fraction of medical papyri that existed, as some papyri quote or allude to unknown texts.[12]
Some papyri appear to have been handbooks for physicians, while others have outlines from lectures, record instructions including lecture notes, or were clinical notebooks owned by students.[13] Many simply provide remedies for diseases, listing numerous drugs available but without including much other information. These drugs are likely to have been from local plants, minerals, and animals, but some may also have been imported, such as lapis lazuli from Afghanistan.[14] A few of the papyri that incorporate magic explain their origins in order to establish authority and authenticity, in certain cases stating that they were found at the foot of a statue of a god.[15] Although many of the texts have been successfully translated, there is still much that is unknown. Some of the vocabulary only occurs in the medical texts, while other words are well known in nonmedical settings but have specific unknown meanings in the medical context.[16]
The Edwin Smith and Ebers Papyri are the most well-known and informative of all the medical papyri, giving a structured method of approaching patient diagnosis and treatment. Both were purchased in 1862 by the American Edwin Smith, who lived in Luxor, Egypt, from 1858–1876 (the Ebers Papyrus was later purchased by Georg Ebers in 1872). They may have come from the same tomb, that of a physician buried in the Theban necropolis on the west bank of the Nile.[17] The Edwin Smith Papyrus dates to circa 1600 BCE (late Middle Kingdom), with most of the language being in Middle Egyptian. It is generally agreed, however, that the original dates to the Old Kingdom (ca. 2600–2500 BCE). This papyrus stands out for its content and approach to medicine, and is often referred to as the surgical papyrus. It focuses on forty-eight cases of mostly traumatic injuries and treatments of the head, face, neck, upper part of the thorax, spine, and arm.[18] It follows empirical understanding, is an instruction book rather than simply a compilation of remedies, and only has one spell. Each medical case follows the same pattern, beginning with the title “knowledge gained from practical experience: examination, diagnosis and prognosis, and treatment.”[19] Physical manipulations, sutures, and bandages are the primary means of treatment of injuries that were likely caused by various types of weapons.[20]
Over time, the Edwin Smith Papyrus became one of the standard reference texts on treating trauma in ancient Egypt and the glosses that were added to fill in omissions attest to its continual utilization.[21] If the Edwin Smith Papyrus is as old as some scholars believe, it contains the earliest known examination of the pulse and details the parallel roles of the physician, the priest of Sekhmet, and magicians. Some scholars propose that the papyrus contains the first description of the circulation of blood. If this is true it means that there was some understanding of this long before the Greek Democritus’ own description in his treatise On Nutrition.[22] After Smith’s death the papyrus was donated to the New York Historical Society and in 1920 the papyrus was given to Egyptologist James Henry Breasted for translation. After a lengthy period of study and analysis, Breasted translated the papyrus. In 1930, he published a historic two-volume edition containing the English translation, with medical notes prepared by physician Arno Luckhardt and an hieroglyphic transcription of the original scroll.
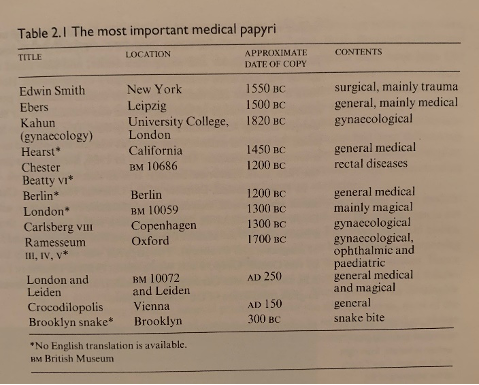
The Ebers Papyrus (circa 1550 BCE) is the longest medical text and is in very good condition (fig. 3).
Figure 3. A section from the Ebers Papyrus (circa 1550 BCE). From the National Library of Medicine at the U.S. National Institute of Health, http://resource.nlm.nih.gov/101436767.
This text is a compilation of original medical texts haphazardly ordered, which makes deciphering references to ailments and treatments difficult, but it nonetheless presents us with a breadth of information. Paragraph 856a notes that the original text was “‘found amongst writings of ancient times in chests of writing material under the feet of Anubis, in Letopolis, in the time of the majesty of the king of Upper and Lower Egypt Den’ (First Dynasty).”[23] This gave the text added ancient authority in its own time (the Berlin Papyrus makes the same statement), as the god Anubis possessed medical knowledge and was patron of embalmers. Unlike the Edwin Smith Papyrus, diseases or symptoms are often assumed, so only a treatment or remedy is listed. Medical issues addressed in this text include those related to the stomach (15 diseases); the anus; the skin (18 diseases); a significant section focuses on the eye (29 diseases); and 21 treatments are provided for cough.[24] There is also a notable section called The Book of Vessels, which focuses on the metu. The metu is generally identified as the blood vessels, ducts, tendons, muscles, and possibly the nerves, although it is uncertain how well the ancient Egyptians understood the nervous system. The metu may transport blood, air, mucus, semen, urine, and disease, acting as canals for substances to flow through. The pulse was taken regularly to make sure the metu vessels were open.[25] The end of the text is more surgical in nature and is our primary source on surgery outside of trauma, listing about 700 drugs and 800 formulas.[26] There are several spells in the text and there are parallels with the Hearst, Berlin, and London papyri.[27]
Another noteworthy medical text is the Kahun gynecological papyrus. This papyrus was found by Flinders Petrie in 1889 in the Fayum area. It dates to circa 1850–1825 BCE, during Amenemhat III’s reign, and is written in hieratic, although the accompanying veterinary text is in hieroglyphic script, which is usually reserved for religious texts. It is in very poor condition, but nonetheless gives us insight into ancient Egyptian’s notions of gynecological issues, including contraception and pregnancy testing. The information does not relate to current gynecological understanding and there is nothing about obstetrics or midwives. Along with this text, there are substantial sections of the Berlin, Carlsberg, Ebers, London, and Ramesseum papyri that address gynecological concerns.[28]
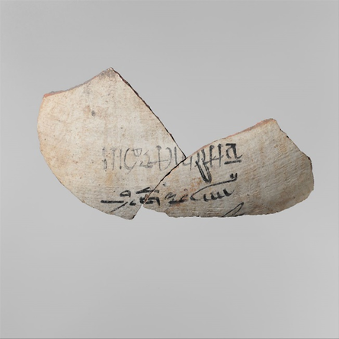
In addition to writing medical knowledge on papyri, physicians also wrote on ostraca, which are potsherds or flakes of mostly white limestone. Due to the material used, ostraca last longer than papyri. Known medical ostraca date from the Amarna Period (Eighteenth Dynasty) to the Roman occupation (30 BCE–395 CE).[29] Medical ostraca were likely used to transmit knowledge and collect treatments in texts. Frequently, medical treatments were listed one after another on these. In general, ostraca were easy to carry and were disposable. As a result, there are probably many medical ostraca missing. Unfortunately, we do not know who specifically used ostraca, whether all physicians did or only physicians of certain levels.
The Medical Profession
While the pharaoh was seen as the supreme healer, his powers were delegated to physicians, priests of Sekhmet and Serqet, and magicians who played critical roles in the process of diagnosing and treating injuries and diseases. Often these roles were intertwined with one other, with some individuals having one or more of these positions. Physicians came from various social classes and the title of physician was held in high regard.
Swnw is usually the ancient Egyptian term translated as doctor or physician (fig. 4).
| Figure 4. Ancient Egyptian hieroglyphic variations of the word swnw. From John F. Nunn, Ancient Egyptian Medicine (Norman: University of Oklahoma Press, 1996). | 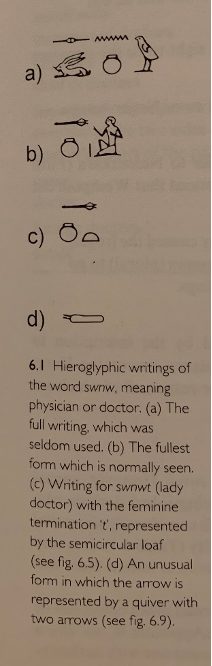 |
This title appears 150 times in tomb biographies, graffiti, stelae, and papyri dating from the Fourth Dynasty (2649–2513 BC) to the Twenty-seventh Dynasty (525–404 BCE). This is linguistically similar to the Egyptian word for pain (swny.t) and for affliction (swn).[30] One of the identifying features of the swnw in the medical papyri is the phrase “placing the hand.”[31] This may have been a way of diagnosing and/or was similar to “the laying on of hands” as we say today as a means of healing.[32] After the Twenty-seventh Dynasty, when Egypt came under Persian rule, swnw came to mean both doctor and embalmer.[33] Furthermore, during the Ptolemaic Period, swnw could mean embalmer as well.[34] Previously, during the Pharaonic period, there may have been limited interactions between physicians and embalmers. Egyptologist Kent Weeks recommends that a more accurate translation of swnw should be “one who treats the ailments of the upper classes,” which reflects the idea that most swnw had connections with the royal court rather than treating ordinary people.[35]
Wab (pure) priests and sau (magicians) were additional healers who used similar healing techniques as swnw. Wab priests and sau are mentioned in the Edwin Smith and Ebers papyri as placing their hand over a patient, demonstrating their participation in healing traumatic injuries and internal ailments. The title wab can refer to even the most novice temple personnel. In the medical context, the title is usually, “wab priest of Sekhmet.” The lioness goddess Sekhmet was both a destructive and healing force. Sau is often translated as magician, but some scholars suggest that a better translation is “protector” or “amulet-man,” although the latter may not be completely accurate either as it implies that the sau only worked with amulets, which is not the case. Sau is often used in connection with Serqet, the scorpion goddess. Like Sekhmet, this goddess also embodied destructive and healing aspects.[36]
The Court physician formed the apex of the medical field.[37] In the Old Kingdom, nearly half of the known doctors and dentists had royal connections. After the Old Kingdom the number of known doctors with a royal connection becomes much fewer. Several swnw also had a priestly title, such as wab priest of Sekhmet, hem netjer (servant of god), or wab nesu (royal priest). Additionally, some swnw were appointed to estates of gods, including that of Amun and Ptah, as well as the “Place of Truth” (the necropolis). [38] Selected physicians were sent to treat miners, workmen, or soldiers, or else were temple physicians, who were at the lowest level of the social ladder and made house visits.[39] Physicians often associated themselves with deities who related to their specialties.[40]
Physician Titles
While most physicians had the title swnw, there were other known related titles, including kherep swnw, meaning the most exalted “controller or administrator of doctors.” Hery swnw and imy-r mean “one with authority over doctors” and “overseer,” respectively, while sehedj or shd swnw is translated as “inspector.” The senior physician was referred to as “Overseer of the House of Health” or “Chief of the House of Secrets,” and smsw swnw meant the “eldest of doctors.”[1] The most widely held special title was wr swnw, meaning “great one” or “chief” physician. Sometimes titles were followed by the geographic limitation of authority, such as Upper or Lower Egypt or both. Many physicians served pharaoh, often having the title swnw per aa, meaning “doctor of the Great House or palace.”
Documents suggest that, much like in modern medicine, ancient Egyptian doctors had specialties.[41] For example, Herodotus famously recorded in his travels to Egypt in about 450 BCE that “medicine is practiced among them on a plan of separation; each physician treats a single disorder, and no more: thus, the country swarms with medical practitioners, some undertaking to cure diseases of the eye, others of the head, others again of the teeth, others of the intestines, and some of those which are not local.”[42] This sentiment is supported by qualifying words relating to body parts following swnw, which have been found on several stelae.[43] In addition, a number of doctors noted that they were also scribes, and some doctors were also dentists. It has been argued that swnw was primarily a physician while surgeons may have been referred to as “great ones of the body” and were mainly wab priests of Sekhmet.[44]
Physicians received years of training at the Peri-Ankh, or “House of Life,” which was either within or attached to a temple and also served as a scriptorium and library where master copies of papyri were likely held.[45] Medicine was a specialty within scribal education.[46] Surgeons received special rudimentary training. It was a science and known as early as 4000 BCE, although the first record of surgical procedures was as early as 2500 BCE.[47] In addition, it appears, based on the papyri, that all physicians were expected to have basic knowledge of all types of medication available.[48] There is indication that medical wisdom was passed down through families, as found on stelae concerning Khay and Huy as well as being documented in the Ebers Papyrus in an obscure passage.[49]
Like other parts of the ancient Near East, such as Mesopotamia, Egypt’s political structure meant that the medical field was well organized, although there was no medical licensure system.[50] Physicians were required to follow strict rules of treatment. One reason for this was that it was deemed that there was nothing to improve upon the existing wisdom of older eras. Physicians were advised to use only the authoritative texts and methods so that their actions would be beyond question.[51] Later, Aristotle wrote that physicians were “warned by the state not to alter a course of treatment until at least four days have passed, or else be subject to legal penalties.”[52] For example, if the physician deviated within those four days he risked the penalty of death if the patient died.
Based on the evidence we have, about 150 physicians are attested to from the Old Kingdom to the Late Period.[53] A few notable physicians are Djer; Imhotep; Amenhotep, son of Hapu; Netjer-hotep; Hesy-ra; Pesehet; Mereuka; Ankh; Ir-en-akhty; Gua and Seni; Renef-seneb; Hery-shef-nakht; Wedja-hor-resnet; Iry; and Pentu. Imhotep (“he who comes in peace”) is perhaps the most well-known (fig. 5).
 Figure 5. Statuette of Imhotep, donated by Padisu, Late Period-Ptolemaic Period (circa 664–30 BCE). Cupreous (copper-containing) metal, 17.9 cm × 5.4 cm × 12.9 cm (7 1/16 × 2 1/8 × 5 1/16 in.). New York Metropolitan Museum of Art, Theodore M. Davis Collection, Bequest of Theodore M. Davis, 1915, 30.8.94.
Figure 5. Statuette of Imhotep, donated by Padisu, Late Period-Ptolemaic Period (circa 664–30 BCE). Cupreous (copper-containing) metal, 17.9 cm × 5.4 cm × 12.9 cm (7 1/16 × 2 1/8 × 5 1/16 in.). New York Metropolitan Museum of Art, Theodore M. Davis Collection, Bequest of Theodore M. Davis, 1915, 30.8.94.He was the royal chamberlain of Pharaoh Djoser of the Third Dynasty and was architect of the Step Pyramid in addition to being a priest, astrologer, and sage. Possibly by the Nineteenth Dynasty (circa 1295–1186 BCE, New Kingdom) and certainly by the Twenty-seventh Dynasty (circa 525–404 BCE, Persian Dynasty), Imhotep was deified as the “son of Ptah,” later replacing Thoth as the chief god of healing.[54] He was the only non-royal to be deified.[55] Miniature statues of Imhotep were sometimes worn as amulets to protect against disease.[56] During the Ptolemaic Period Imhotep was often identified with Asklepios, the ancient Greek god of medicine, but it is not apparent if Imhotep ever held the title swnw.[57]
Hesy-ra, a contemporary of Imhotep, is considered the first documented doctor in the world (circa 2650 BCE), working during Djoser’s reign. He held several titles, including wer ibeh swnw, “chief of dentists and doctors.”[58] According to a stela found in Akhet-hotep’s Fifth or Sixth Dynasty tomb (circa 2494–2181 BCE, Old Kingdom), Pesehet is possibly the first female physician, or at least the first female overseer, of doctors. She held the titles imy-r swnwt, which could be read “[female] overseer of the female doctors,” and imy-r hem-ka, “overseer of the funerary priest.”[59] While she held the title of overseer, this does not necessarily mean she was a doctor herself. Pesehet remains the only attested female physician in ancient Egypt.[60] Hery-shef-nakht of the Twelfth Dynasty (circa 1985–1795 BCE, Middle Kingdom) uniquely held triple qualification as wer swnw, wab priest of Sekhmet, and overseer of magicians. These titles were recorded in the Ebers Papyrus. He also held the important title wer swnw n nesu, chief of the king’s physicians.[61] Iri, a Sixth Dynasty physician, was referred to as the Keeper of the Royal Rectum and “one understanding the internal liquids” and was possibly the pharaoh’s enema expert.[62]
Ancient Egyptian physicians were well known in neighboring countries. They were regularly requested by the Hittite court.[63] For example, Rameses II was asked to send a physician to the Hittite court “to prepare herbs for Karunta, King of the land of Tarhuntas,” according to an Akkadian text about Pariamakhu.[64] Egyptian doctors were sent to dislodge a possessing demon, to heal the Hittite king’s eye, and “to provide the king’s vassals ‘with all sorts of prescriptions.’”[65] Rameses II also wrote, “They will bring to you all the very good remedies which are here in Egypt, and which I allowed in friendly fashion to go to you in order to help you.”[66] Another request was made in which Neb-amen, a New Kingdom physician, received gifts for assisting a Syrian prince. Homer’s Odyssey also references ancient Egyptian medicine, and Herodotus remarked that before the Persian invasion, King Cyrus sent items to Pharaoh Ahmose II (Amasis) “for the services of the best ophthalmologist in Egypt.”[67] Foreign physicians were also allowed to practice medicine in Egypt, as indicated by four Babylonian physicians in New Kingdom records.[68] The Greeks expressed admiration for Egyptian medicine, specifically the effectiveness of their drugs.[69] In turn, there is evidence that Egyptian physicians adopted medical concepts from contact with peoples in the Levant, most notably during the Eighteenth Dynasty and the Ramesside Period (Nineteenth Dynasty). For example, the Nineteenth Dynasty London Medical Papyrus incorporates seven incantations in two different languages; six are in Northwest Semitic dialects and written in syllabic Egyptian script, while one is in the Cretan language, using syllabic Egyptian script. These prescriptions were accepted into Egyptian medical practice as legitimate remedies rather than being marginalized. Another example is a Cretan spell against an “Asiatic disease” using an Egyptian methodology from the Eighteenth Dynasty Hearst Medical Papyrus to treat the ailment.[70]
Ailments, Injuries, and Treatments
Snake and scorpion bites, eye diseases, and gastrointestinal issues were among the most frequently treated ailments. Pneumonia and silicosis (inhaling dust particles), parasitic diseases, typhoid, dysentery, smallpox, and diarrhea were other common ailments.[71] Although they believed that people were born healthy, ancient Egyptians believed that their well-being was endangered by both earthly and supernatural forces, such as through intestinal putrefaction or malignant deities entering through bodily openings and consuming vital parts of the interior of the body. Supernatural origins of disease “could function as a form of punishment from the gods, a reminder of one’s social obligation or an outright attack by a malicious or capricious entity.”[72] Particularly unpleasant remedies sometimes were prescribed that were intended to rid the body of a malignant spirit.[73] Good health was linked with living correctly, which included being at peace with the gods and spirits, as well as the deceased.[74] It was thought that illness was due to an imbalance that could subsequently be brought back to equilibrium through prayers, spells, and rituals.
It is clear from the Edwin Smith and Ebers papyri that the ancient Egyptians had a rudimentary understanding of the cardiovascular system, seeing this as a network of vessels (metu) coming from the heart and going through the body to the organs and other body parts. The heart was the center of the system, where “the metu delivered and received.”[75] This system involved the movement throughout the body of air, water, blood, and bodily waste, termed as wekhedu. Wekhedu was a distinct focus of the ancient Egyptians.[76] The accumulation of bodily waste sometimes appeared as pus in wounds or blisters as wekhedu worked through the blood system. Physicians sought to treat this by keeping wounds clean and bandaged with honey and copper salts. Physicians advocated purging one’s body and using enemas and emetics in order to keep wekhedu from accumulating. Enemas had a divine origin as ancient Egyptians believed that Thoth invented them.[77]
It is evident from the Edwin Smith Papyrus that the brain was the location “of the nervous control of the body” and that paralysis could be because of a brain injury.[78] The ancient Egyptians had an extensive knowledge about the skull, brain, jaw, and face, in particular. This was due in part to traumatic injuries that often occurred from industrial accidents, warfare, or animal bites.[79] Fractures were frequent injuries. Consequently, the Egyptians had an extensive set of words describing various types of fractures, including more complicated ones.[80]
In terms of treatment, it was often stated in the Edwin Smith and Ebers papyri that the doctor would either treat, “contend with,” or not treat.[81] The options were based on the level of the physician’s confidence that the injury was treatable. If a patient could not be treated, he or she was still given care and kept comfortable until death.[82]
Views on the sources and nature of diseases ranged widely and medical classifications were made based on symptoms rather than diseases. Traumatic injuries had an obvious origin and therefore a sure means of diagnosis and treatment with some predictable outcome.
This includes the belief that objects could be infused with a life-force or spirit, allowing the object to act against an individual, thus was the cause of the injury because the object readjusted maat.[83] Conversely, internal issues, such as heart disease and lung ailments, had unpredictable outcomes as the source of illness was not always apparent. In these cases, reliance on incantations, spells, and amulets was common, sometimes in combination with drugs. If it was believed that there was a supernatural origin of the disease, such as a malign deity, the supernatural (benign deities) would be relied upon to cure the ailment. Many deities were invoked to prevent or cure diseases or attacks by dangerous animals.[84] Incantations often took the form of directly addressing the disease or disease-demon. Incantations or prayers were also meant to reinforce the effectiveness of remedies and often were related to specific diseases and drugs.[85] They were infused with heka, which involved the component of speech.[86] Egyptians thought that the “divine creative word and magical energy” could turn ideas into reality and therefore negate or turn away negative forces.[87] Often, spells or incantations had a “sympathetic” role; therefore, they would have been pragmatic and rational to the ancient physician.[88]
Amulets were also worn as a means of addressing health care. Many amulets resembled living creatures (human or animal) or specific body parts, with the intent of the wearer assimilating the desired characteristic, such as strength or sharp eyesight. A number of people also wore amulets to protect against harm, such as animal bites.[89] It was thought that the material the amulet was made of and the shape of it provided protection and healing for the wearer. Even substances that came in contact with amulets were considered to have a healing effect.[90] Amulets have been used by many people across the centuries and cultures. People still wear them today, believing that certain objects, whether they are of natural material or human-made, have power from a greater force, from a religious connection, or through the way the object was created. A rabbit’s foot or other good-luck charms are such examples.
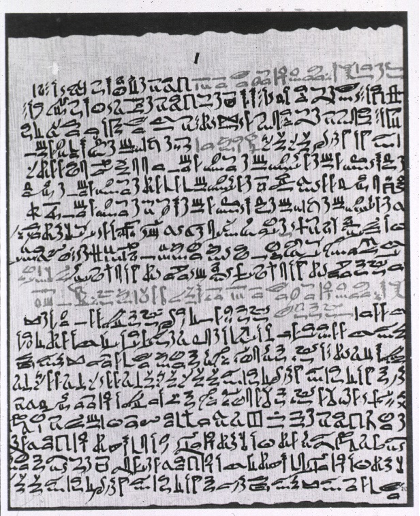
Prescriptions made from animals, minerals, and vegetable substances were a regular means of treating various types of illnesses and injuries. The ancient Egyptian pharmacopeia was quite rich, although many of the terms have not yet been translated.[91] The efficacy of various drugs was not always evident, since multiple drugs were often utilized simultaneously, with several elements involved, while other times drugs were used in tandem with magic. Water, alcohol (beer and wine), oil, honey, and milk were part of preparing various types of prescriptions (fig. 6).[92]
Figure 6. Pharmaceutical jar, Saite Period, Twenty-sixth Dynasty (570–526 BCE). The inscription lists the contents of the jar as “Special ointment of the Manager of the Red-Crown Enclaves and Chief Physician, Harkhebi.” The man who owned the jar likely lived in the town of Buto in the Nile Delta. The “Red-Crown Enclaves” was an ancient area in Buto. Travertine (Egyptian alabaster), 47 × 34 cm (18 1/2 × 13 3/8 in.). New York Metropolitan Art Museum, Rogers Fund, 1942, 42.2.2.
Drugs were administered in five ways: orally, rectally, vaginally, by external application, and by fumigation. They were given in the form of cakes, suppositories, enemas, mouth rinses, tablets, drops, ointments, or special baths.[93] Often prescriptions would be made based on the patient’s age and weight.[94] Physicians also recited incantations while preparing or administering prescriptions.[95]
Drugs made from animals include honey, milk, excrement, blood, urine, placenta, bile, animal fat, meat, and liver and other internal organs. Honey was an especially beneficial element for its antibacterial and antifungal properties, as well as being a flavorful additive to other drugs (fig. 7).
Figure 7. Fragment of a jar with a label identifying the contents as honey. The script is in hieratic, which is written right to left. The sign at the beginning of the second line represents a bee, the symbol used for the word “honey.” New Kingdom, Eighteenth Dynasty (1390–1352 BCE). Pottery and ink, 8.5 x 15.3 × 0.7 cm (3 3/8 × 6 × 1/4 in.). New York Metropolitan Art Museum, Rogers Fund, 1917, 17.10.12.
Honey was used both internally, including helping with cough, and externally, for various types of wounds.[96] This is the case today as well. Honey is still used to help reduce coughs and sooth sore throats. It is also beneficial in healing wounds, including burns and leg ulcers, because of its antibacterial and anti-inflammatory properties. For this reason, it may also help with skin grafts.[97] Milk was mainly used to make it easier to swallow other ingredients, although it was sometimes used as an enema or applied to skin, eyes, or ears.[98] Like honey, it also helped with respiratory ailments and throat irritations. Animal fat was utilized to make a greasy ointment, but also to convey the meaningful animal characteristics, such as strength.[99] For certain wounds, applying a bandage with fresh meat on the first day was general practice. In subsequent days, bandages with honey and oil or resin would be applied, which helped the healing process.
Some mineral-based drugs that were used include natron, common salt, malachite, lapis lazuli, imru, and gypsum. Natron was particularly beneficial in drawing out fluid and reducing swelling and was often applied with bandages. Malachite was the base for green eye paint and was often used for treating eye diseases, which were widespread due to flies, dust, and sand. Malachite is a natural antibacterial and was used in cases to treat burns or inflammation. However, it is unclear if the ancient Egyptians recognized this property or if they were more influenced by the decorative elements of the mineral.
The ancient Egyptians took advantage of the plants and herbs available to them, including onions, mint, lettuce, barley, acacia, dates, willow, dill, aloe vera, frankincense, garlic, mustard seeds, and linseed, among others. Aloe vera is one plant we still use to help soothe sunburns and other skin ailments. We also mint or peppermint today to help with stomach issues. Unfortunately, there is difficulty in positively identifying some of the plant species that were used. Reasons for this are that the disease for which the remedy was created cannot be translated or is otherwise unknown; in a few cases it is unknown which part of the plant was added, or we may not know the fullness of the pharmacological effect of the plant. Some plants may now be extinct or have disappeared from the Nile Valley, which also hinders researchers in determining the plant species that were used.[100] Cannabis was known by the ancient Egyptians, including using hemp to make rope. It infrequently appears in the medical papyri and was administered by mouth, rectum, vagina, fumigation, on bandaged skin, and applied to the eyes. It is unknown if the Egyptians understood the effects of the plant on the nervous system.[101] Alcohol was likely the customary means of alleviating pain, just as it has been used in the centuries since.
Nearly a quarter of the listed prescriptions in the Ebers Papyrus were for gastrointestinal issues. As previously commented, the bowels were a specific focus for the ancient Egyptians at all levels of society, as they believed that a certain toxin (wekhedu) originated there, which could then spread to the rest of the body and cause aging, disease, and death.[102] They practiced purging themselves on a regular basis in order to keep their bodies healthy (Herodotus noted that this occurred for three days each month).[103] Castor oil, senna, and colocynth were often consumed for this process, while earth almonds and tiger nuts were also regularly eaten. Wormwood and pomegranate were effective in treating intestinal parasites.
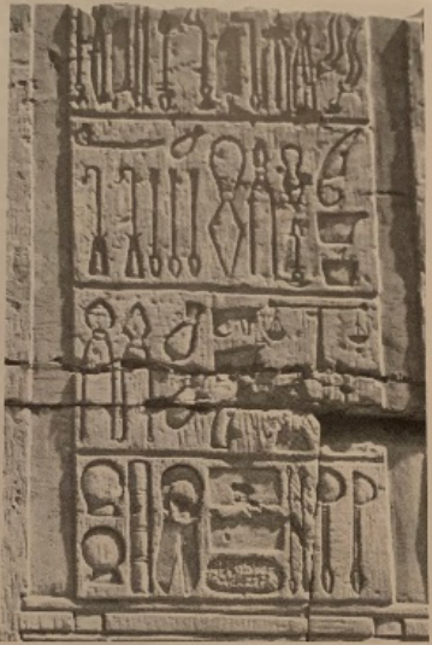
There currently is not much documentation of surgery beyond simple procedures including removing tumors, closing wounds, or treating traumatic injuries such as fractures. There are only a few examples of human remains that show that the ancient Egyptians knew of trephination to relieve swelling of the brain.[104] Wounds were often either closed with linen sutures, as observed in seven cases in the Edwin Smith Papyrus, or bandaged with linen.[105] Surgery deep inside the body was generally not practiced because of the lack of an anesthetic.[106] Some surgical instruments referenced in the medical papyri are lancets, tweezers, drills, hook-like instruments, retractors, and dental tools (fig. 8).
Figure 8. Image of medical instruments chiseled on the inner part of the northern section of the outer enclosure wall of the temple of Kom Ombo (Roman era). Kom Ombo is north of Aswan in southern Egypt. From John F. Nunn, Ancient Egyptian Medicine (Norman: University of Oklahoma Press, 1996).
Bronze was initially widely implemented but later copper was the preferred metal.
Snakes were much dreaded in ancient Egypt. While the Edwin Smith Papyrus does not address how snake bites were treated and the Ebers Papyrus only minimally addresses this, the Brooklyn Museum Papyri focuses on this subject. The extant copy of the text dates to circa 6th-4th century BCE, although the original may date as early as the Old Kingdom.[107] The papyri identify at least twenty-one snakes and one chameleon. It also provides a brief description of the effects of the different types of snake bites, along with the prognosis. Care included local treatment of the bite, drugs (mainly herbal), and incantations. Many of these treatments intended to address pain and swelling as opposed to preventing the general absorption of the venom. There are several suggestions of applying bandages, which would have helped with applying localized drugs. Onion was one of the primary ingredients for treating bites, which was often part of a compound with salt and sweet beer, and at times was utilized along with incantations. Emetics were also prescribed, as the theory was to expel the venom through vomiting. The kherep priests of Serqet were the main healers in preventing and treating snake bites as well as scorpion stings.[108]
Ancient Egypt’s Influence on Greek Medicine
Not long after Alexander the Great invaded Egypt in 332 BCE, the famous Alexandrian medical school was established, which had a great impact during the Ptolemaic, Roman, and Coptic periods. Many Greek physicians studied there, including Herophilus and Galen. Pliny the Elder, the Roman naturalist, asserted that the art of medicine may have been invented by the Egyptians.[109] Scholars have long debated the extent to which the Egyptians may have influenced ancient Greek medicine.
The following is what some scholars claim as being among the contributions. The Greek physician Herophilus, who studied in Alexandria, adopted the technique of pulse-taking as developed by the Egyptians. In addition, the practice of mummification allowed for anatomical dissection, which was otherwise taboo in ancient Greece. The Pre-Alexandrian Hippocratic Corpus illustrates parallels with Egyptian ideas and practices, such as birth prognoses adapted from pregnancy texts found in the Kahun, Carlsberg, and Berlin papyri, as well as disorders of the womb.[110] Some of the Greek gynecological, and possibly surgical, techniques may also be attributed to ancient Egyptians.[111] A few Egyptian terms were also adopted into Greek, such as that for migraine.[112] The four humors in Greek thinking may have also first come from Egypt.[113]
In addition, we know that the Greeks imitated and further developed the practice of empirical examination of patients, including diagnosis and prognosis.[114] The practice of incubation (sleeping in a sacred area with the purpose of experiencing divine dreams or healing) may also have originated with the Egyptians.[115] There is textual evidence that this practice existed at Deir el-Medina during the New Kingdom, circa 1200 BCE, and that temples at Sais and Heliopolis were well-known medical centers in the Middle Kingdom, circa 1900 BCE.[116]
One of the most noteworthy ancient Egyptian contributions to Greek, and later Roman, medicine is pharmaceuticals. The symbol for prescription, Rx, is Latin for “recipe,” meaning “take,” and may have originated from the Eye of Horus (fig. 9), which was an especially significant component of ancient Egyptian medicine, as it was believed that it had power to heal and protect.
Figure 9. Stamp seal in the shape of Wedjat-Eye (Eye of Horus), New Kingdom, Eighteenth Dynasty (1400–1390 BCE). Steatite (glazed), 1.7 × 1.1 × 0.6 cm (11/16 × 7/16 × 1/4 in.). New York Metropolitan Art Museum, gift of Helen Miller Gould, 1910, 10.130.208.
It also served to measure prescriptions, as the mathematical proportions of the eye were used to determine the amount of ingredients in medicines. The eye was divided into six parts related to the six senses: touch, taste, thought, hearing, sight, and smell.[117] In addition, many drugs and vegetable substances termed “Egyptian” played a prominent role in Greek and Roman medicine, as found in Greek medical works such as the Hippocratic Corpus and in the works of Herophilos, Dioscurides, Galen, and Pliny. The Odyssey also refers to Helen of Troy dispensing a drug to soothe her guest, where it is said to have been a gift from an Egyptian woman, and she praises Egyptian physicians as being “knowledgeable beyond all humans.”[118] Pharmaceutical contributions include natron, aloe, chicory, alum, beans, castor oil, comfrey, pomegranate, saffron, and other oils and perfumes. The most popular was natron, as it is a naturally occurring soda that is used for cleansing purposes. The administration of drugs was also influenced by the Egyptians. Greek physicians at the Alexandrian medical school were the first to quantify specific ingredients in remedies, mimicking the precision of the Egyptians. One markedly influential prescription ingredient was the “milk of a woman who has borne a male child,” which was “sympathetically evoking the curative milk of Isis after the birth and injury of [her son] Horus” (fig. 10).
Figure 10. Isis and the infant Horus, circa 300 BCE, Ptolemaic Kingdom (332 BCE–30 CE). Bronze and wood, 16.51 cm (6.5 in.). Spencer Museum of Art, University of Kansas, gift of Dr. Franklin D. Murphy, 1956.0029.
This element can be found several times in Egyptian texts and later was recommended in the Hippocratic Corpus, by Pliny and Dioscorides, in Coptic medicine, and in British herbals from the twelfth through seventeenth centuries. Castor oil was another prescribed drug that is still used today.[119] Conversely, in later Egyptian medical papyri new drugs appear, and while they are transcribed in Egyptian, they originated from someplace else.[120]
Chronology of ancient Egyptian dynasties, notable physicians, and medical papyri. From John F. Nunn, Ancient Egyptian Medicine (Norman: University of Oklahoma Press, 1996).
Bibliography
Aboelsoud, N. H. “Herbal Medicine in Ancient Egypt.” Journal of Medicinal Plants Research 4, no. 2 (2010): 82–86.
Allen, James P. “The Art of Medicine in Ancient Egypt.” In The Art of Medicine in Ancient Egypt. New York: The Metropolitan Museum of Art, 2005, 9–12.
Carrick, Paul. Medical Ethics in the Ancient World. Washington: Georgetown University Press, 2001.
Escolano-Poveda, Marina. “Demotic: Opening New Windows into the Understanding of Egyptian History and Culture.” ARCE, American Research Center in Egypt. October 20, 2020. https://www.arce.org/resource/demotic-opening-new-windows-understanding-egyptian-history-and-culture#:~:text=The%20term%20%E2%80%9CDemotic%E2%80%9D%20refers%20to,language%20of%20the%20New%20Kingdom.
Gross, Charles. “From Imhotep to Hubel and Wiesel: The Story of Visual Cortex.” In Brain, Vision, Memory: Tales in the History of Neuroscience. Cambridge, MA: MIT Press, 1998, 1–90.
Horstmanshoff, H. F. J., and Marten Stol, eds. Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine. Leiden: Brill, 2004.
Longrigg, James. Greek Rational Medicine: Philosophy and Medicine from Alcmaeon to the Alexandrians. London: Routledge, 1993.
Meo, Sultan Ayoub, Saleh Ahmad Al-Asiri, Abdul Latief Mahesar, and Mohammad Javed Ansari. “Role of Honey in Modern Medicine.” Saudi Journal of Biological Sciences 24 no. 5 (2017): 975–78.
Mininberg, David T. “The Legacy of Ancient Egyptian Medicine.” In The Art of Medicine in Ancient Egypt. New York: The Metropolitan Museum of Art, 2005, 9–12.
Nicolaides, Angelo. “Assessing Medical Practice and Surgical Technology in the Egyptian Pharaonic Era.” Medical Technology SA 27, no. 1 (2013): 19–25.
Nunn, John F. Ancient Egyptian Medicine. Norman: University of Oklahoma Press, 1996.
Porter, Roy. The Greatest Benefit to Mankind: A Medical History of Humanity. New York: W.W. Norton Co., 1997.
Ritner, Robert K. “Innovations and Adaptations in Ancient Egyptian Medicine.” Journal of Near Eastern Studies 59, no. 2 (2000): 107–17.
Saber, Aly. “Ancient Egyptian Surgical Heritage.” Journal of Investigative Surgery 23, no. 6 (2010): 327–34.
Saunders. J. B. de C. M. The Transitions from Ancient Egyptian to Greek Medicine. Lawrence, KS: University of Kansas Press, 1963.
“Snakebite Papyrus.” Brooklyn Museum. https://www.brooklynmuseum.org/opencollection/objects/124173.
Sullivan, Richard. “A Brief Journey into Medical Care and Disease in Ancient Egypt.” Journal of the Royal Society of Medicine 88, no. 7 (1995): 141–45.
Zucconi, Laura M. “Medicine and Religion in Ancient Egypt.” Religion Compass 1, no. 1 (2007): 26–37.
Suggested Further Reading
Ghaliounghui, Paul. The House of Life: Magic and Science in Ancient Egypt. 2nd ed. Amsterdam: B.M. Israël, 1973.
Ghaliounghui, Paul. The Physicians of Pharaonic Egypt. Cairo: Al-Ahram Center for Scientific Translations, 1983.
Grapow, Herman, and Hildegard von Deines. Grundriss der Medizin der Alten Ägypter. Berlin: Akademie-Verlag, 1954.
Halioua, Bruno, and Bernard Ziskind. Medicine in the Days of the Pharaohs. Trans. M.B. DeBevoise. Cambridge, MA: The Belknap Press of Harvard University Press, 2005.
Jonckheere, Frans. Les Médicines de l’Egypte Pharaonique: Essai de Prosopographie. Brussels: Éditions de la Fondation Éqyptologique, 1958.
Laskaris, Julie. The Art Is Long: On the Sacred Disease and the Scientific Tradition. Leiden: Brill, 2002.
Lefebvre, Gustave. Essai sur la Médecine Égyptienne de l’Époque Pharaonique. Paris: Presses
Universitaires de France, 1956.
Majno, Guido. The Healing Hand: Man and Wound in the Ancient World. Cambridge, MA: Harvard University Press, 1975.
Manniche, Lise. An Ancient Egyptian Herbal. Austin: University of Texas Press, 1989.
Saba, Magdi M., Hector O. Ventura, Mohamed Saleh, and Mandeep R. Mehra. “Ancient Egyptian Medicine and the Concept of Heart Failure.” Journal of Cardiac Failure 12, no. 6 (2006): 416–21.
Westendorf, Wolfhart. Handbuch der altägyptischen Medizin. Leiden: Brill, 1999.
[1]. Laura M. Zucconi, “Medicine and Religion in Ancient Egypt,” Religion Compass 1, no. 1 (2007): 26.
[2]. Zucconi, “Medicine and Religion,” 27.
[3]. Zucconi, “Medicine and Religion,” 28.
[4]. Zucconi, “Medicine and Religion,” 28.
5. John F. Nunn, Ancient Egyptian Medicine (Norman, OK: University of Oklahoma Press, 1996), 115.
[6]. Zucconi, “Medicine and Religion,” 36; and Roy Porter, The Greatest Benefit to Mankind: A Medical History of Humanity (New York: W.W. Norton Co., 1997), 49.
[7]. Richard Sullivan, “A Brief Journey into Medical Care and Disease in Ancient Egypt,” Journal of the Royal Society of Medicine 88, no. 7 (1995): 141–42.
[8]. Angelo Nicolaides, “Assessing Medical Practice and Surgical Technology in the Egyptian Pharaonic Era,” Medical Technology SA 27, no. 1 (2013): 19.
[9]. Zucconi, “Medicine and Religion,” 26.
[10]. Nunn, Ancient Egyptian Medicine, 23, 24, 39.
[11]. Marina Escolano-Poveda, “Demotic: Opening New Windows into the Understanding of Egyptian History and Culture,” ARCE, American Research Center in Egypt, October 20, 2020, https://www.arce.org/resource/demotic-opening-new-windows-understanding-egyptian-history-and-culture#:~:text=The%20term%20%E2%80%9CDemotic%E2%80%9D%20refers%20to,language%20of%20the%20New%20Kingdom.
[12]. Nunn, Ancient Egyptian Medicine, 24; and Robert K. Ritner, “Innovations and Adaptations in Ancient Egyptian Medicine,” Journal of Near Eastern Studies 59, no. 2 (2000): 108.
[13]. Rosalie David in H. F. J. Horstmanshoff and Marten Stol, eds., Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine (Leiden: Brill, 2004), 140.
[14]. Nunn, Ancient Egyptian Medicine, 138.
[15]. Nunn, Ancient Egyptian Medicine, 104.
[16]. Nunn, Ancient Egyptian Medicine, 25, 68.
[17]. Nunn, Ancient Egyptian Medicine, 30.
[18]. James P. Allen, “The Art of Medicine in Ancient Egypt,” in The Art of Medicine in Ancient Egypt (New York: Metropolitan Museum of Art, 2005), 11.
[19]. Nunn, Ancient Egyptian Medicine, 26–30; and Allen, “The Art of Medicine in Ancient Egypt,” 9.
[20]. Zucconi, “Medicine and Religion,” 27; and Allen, “The Art of Medicine in Ancient Egypt,” 9.
[21]. Nunn, Ancient Egyptian Medicine, 26–30.
[22]. Sullivan, “A Brief Journey,” 141.
[23]. Nunn, Ancient Egyptian Medicine, 31, 38; and J. B. de C. M. Saunders, The Transitions from Ancient Egyptian to Greek Medicine (Lawrence, KS: University of Kansas Press, 1963).
[24]. Porter, The Greatest Benefit, 48.
[25]. Zucconi, “Medicine and Religion,” 28.
[26]. Porter, The Greatest Benefit, 48.
[27]. The majority of the information in this paragraph comes from Nunn, Ancient Egyptian Medicine, 30–34.
[28]. All Information in this paragraph comes from Nunn, Ancient Egyptian Medicine, 34–35.
[29]. Nunn, Ancient Egyptian Medicine, 41.
[30]. Zucconi, “Medicine and Religion,” 35.
[31]. Nunn, Ancient Egyptian Medicine, 115.
[32]. Nunn, Ancient Egyptian Medicine, 115.
[33]. Nunn, Ancient Egyptian Medicine, 115, 134.
[34]. Nunn, Ancient Egyptian Medicine, 44.
[35]. Robert Arnott in H. F. J. Horstmanshoff and Marten Stol, eds., Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine (Leiden: Brill, 2004), 156n7.
[36]. Information in this paragraph from Zucconi, “Medicine and Religion,” 34.
[37]. Porter, The Greatest Benefit, 49.
[38]. The majority of the information in this paragraph comes from Nunn, Ancient Egyptian Medicine, 116–118, 120.
[39]. Nicolaides, “Assessing Medical Practice,” 21.
[40]. Sullivan, “A Brief Journey,” 142.
[41]. Nunn, Ancient Egyptian Medicine, 11.
[42]. Paul Carrick, Medical Ethics in the Ancient World (Washington: Georgetown University Press, 2001), 15. Porter also cites a similar quote; see The Greatest Benefit, 49.
[43]. Nunn, Ancient Egyptian Medicine, 119.
[44]. Nicolaides, “Assessing Medical Practice,” 20; and Nunn, Ancient Egyptian Medicine, 119.
[45]. Nicolaides, “Assessing Medical Practice,” 21; and David, Magic and Rationality, 138.
[46]. David T. Mininberg, “The Legacy of Ancient Egyptian Medicine,” in The Art of Medicine in Ancient Egypt (New York: Metropolitan Museum of Art, 2005), 13.
[47]. Nicolaides, “Assessing Medical Practice,” 19, 22.
[48]. Nicolaides, “Assessing Medical Practice,” 21.
[49]. Nunn, Ancient Egyptian Medicine, 130–131.
[50]. Porter, The Greatest Benefit, 50.
[51]. Nicolaides, “Assessing Medical Practice,” 21.
[52]. Carrick, Medical Ethics, 72.
[53]. Ritner, “Innovations and Adaptations,” 116.
[54]. Nunn, Ancient Egyptian Medicine, 122; and Nicolaides, “Assessing Medical Practice,” 20.
[55]. Nicolaides, “Assessing Medical Practice,” 20.
[56]. Charles Gross, “From Imhotep to Hubel and Wiesel: The Story of Visual Cortex,” in Brain, Vision, Memory: Tales in the History of Neuroscience (Cambridge, MA: MIT Press, 1998), 5.
[57]. Nunn, Ancient Egyptian Medicine, 122; and Allen, “The Art of Medicine,” 12.
[58]. Nunn, Ancient Egyptian Medicine, 124.
[59]. Nunn, Ancient Egyptian Medicine, 124.
[60]. Ritner, “Innovations and Adaptations,” 117; and Porter, The Greatest Benefit, 49.
[61]. Nunn, Ancient Egyptian Medicine, 128.
[62]. Porter, The Greatest Benefit, 49; and Nicolaides, “Assessing Medical Practice,” 21.
[63]. Ritner, “Innovations and Adaptations,” 111; and Arnott, Magic and Rationality, 169.
[64]. Nunn, Ancient Egyptian Medicine, 131.
[65]. Ritner, “Innovations and Adaptations,” 112.
[66]. Ritner, “Innovations and Adaptations,” 112.
[67]. Nunn, Ancient Egyptian Medicine, 132; and James Longrigg, Greek Rational Medicine: Philosophy and Medicine from Alcmaeon to the Alexandrians (London: Routledge, 1993), 228n2.
[68]. Most information in this paragraph comes from Nunn, Ancient Egyptian Medicine, 131–32.
[69]. Carrick, Medical Ethics, 15.
[70]. Ritner, “Innovations and Adaptations,” 111.
[71]. Nicolaides, “Assessing Medical Practice,” 20.
[72]. Zucconi, “Medicine and Religion,” 20.
[73]. David, Magic and Rationality, 141.
[74]. Porter, The Greatest Benefit, 49.
[75]. Nicolaides, “Assessing Medical Practice,” 21.
[76]. Ritner, “Innovations and Adaptations,” 114.
[77]. Porter, The Greatest Benefit, 49.
[78]. David, Magic and Rationality, 144.
[79]. Nunn, Ancient Egyptian Medicine, 50.
[80]. Nunn, Ancient Egyptian Medicine, 57.
[81]. Nunn, Ancient Egyptian Medicine, 114.
[82]. Carrick, Medical Ethics, 74.
[83]. Zucconi, “Medicine and Religion,” 30.
[84]. Nunn, Ancient Egyptian Medicine, 96.
[85]. Nunn, Ancient Egyptian Medicine, 105.
[86]. Zucconi, “Medicine and Religion,” 32.
[87]. David, Magic and Rationality, 134.
[88]. Ritner, “Innovations and Adaptations,” 113.
[89]. Nunn, Ancient Egyptian Medicine, 110.
[90]. Allen, “The Art of Medicine,” 10.
[91]. Nunn, Ancient Egyptian Medicine, 144.
[92]. Nunn, Ancient Egyptian Medicine, 139–40.
[93]. Nicolaides, “Assessing Medical Practice,” 21.
[94]. Nicolaides, “Assessing Medical Practice,” 22; and N. H. Aboelsoud, “Herbal Medicine in Ancient Egypt,” Journal of Medicinal Plants Research 4, no. 2 (2010): 84.
[95]. Aboelsoud, “Herbal Medicine in Ancient Egypt,” 82.
[96]. Nunn, Ancient Egyptian Medicine, 148.
[97]. Sultan Ayoub Meo, Saleh Ahmad Al-Asiri, Abdul Latief Mahesar, and Mohammad Javed Ansari, “Role of Honey in Modern Medicine,” Saudi Journal of Biological Sciences 24 no. 5 (2017): 977.
[98]. Nunn, Ancient Egyptian Medicine, 148.
[99]. Nunn, Ancient Egyptian Medicine, 149–50.
[100]. Nunn, Ancient Egyptian Medicine, 151.
[101]. Nunn, Ancient Egyptian Medicine, 156.
[102]. Nunn, Ancient Egyptian Medicine, 158.
[103]. Porter, The Greatest Benefit, 50.
[104]. Nunn, Ancient Egyptian Medicine, 169.
[105]. Nunn, Ancient Egyptian Medicine, 171 and 173; and Mininberg, “The Legacy of Ancient Egyptian Medicine,” 14.
[106]. Nicolaides, “Assessing Medical Practice,” 22.
[107]. Nunn, Ancient Egyptian Medicine, 183; and “Snakebite Papyrus,”
Brooklyn Museum, https://www.brooklynmuseum.org/opencollection/objects/124173.
[108]. All information in this paragraph is from Nunn, Ancient Egyptian Medicine, 188–89, 99–100.
[109]. Longrigg, Greek Rational Medicine, 229n17.
[110]. Longrigg, Greek Rational Medicine, 11.
[111]. Longrigg, Greek Rational Medicine, 10.
[112]. Most information in this paragraph is from Ritner, “Innovations and Adaptations,” 115–16.
[113]. Carrick, Medical Ethics, 15–16.
[114]. Carrick, Medical Ethics, 15.
[115]. Longrigg, Greek Rational Medicine, 10.
[116]. David, Magic and Rationality, 143.
[117]. Aly Saber, “Ancient Egyptian Surgical Heritage,” Journal of Investigative Surgery 23, no. 6 (2010): 333.
[118]. Longrigg, Greek Rational Medicine, 10; and Arnott, Magic and Rationality, 183.
[119]. Much of the information in this paragraph, including the quote about milk, is from Ritner, “Innovations and Adaptations,” 116.
[120]. David, Magic and Rationality, 145.