2 Chapter 2: Causes of Death and Disease in the United States
Brandye Nobiling

Chapter Objectives:
- Compare and contrast leading causes of death in the US
- Define key epidemiology terms: endemic, epidemic, pandemic, prevalence rate, incidence rate, and years of potential life lost
- Define and exemplify the three levels of prevention
- Identify and apply the epidemiological triad to disease causation
- Identify the links in the chain of infection and how the links can be broken
- Identify and apply the multi-causation model to disease causation
- Analyze factors that contributed to the shift in leading causes of death over the past hundred years
- Recognize how Healthy People prioritizes leading causes of death in its framework
Introduction
Chapter One outlined specific diseases that led to morbidity and mortality throughout history as well as discussed various technologies that led to changes in disease causation. In this chapter, we will explore the leading causes of death and disease in more detail to better understand where the focus is in public health today in the United States. Table 2 outlines the leading causes of death in 1900 as well as today.
Table 2. Leading Causes of Death – Then and Now
| 1900 | Today |
| 1). Pneumonia (all types) and influenza | 1). Heart disease |
| 2). Tuberculosis (all forms) | 2). Cancer |
| 3). Diarrhea, enteritis, and ulceration of the intestines | 3). COVID-19 |
| 4). Heart disease | 4). Unintentional injuries |
| 5). Stroke | 5) Stroke |
The table above lists the leading causes of death in the United States in 1900 as well as today for all races, sexes, and ages. In 1900 there was a tie between pneumonia and influenza for the number one leading cause of death. These were followed by tuberculosis, diarrhea (also referred to as dysentery), heart disease, and stroke. The first three leading causes of death (pneumonia, influenza, and tuberculosis) are infectious diseases that are transmitted from person-to-person contact, and tend to have a sudden onset, also called an acute onset. The condition in the number three spot, dysentery, usually was associated with cross-contamination during food preparation and improper sanitation. It isn’t until the latter end of the list that heart disease and stroke – common leading causes of disease today – make an appearance. And cancer, the second leading cause of death today, is not on the list at all. It’s not until 1921 that cancer appears in the top five leading causes of death.
With the exception of unintentional injuries and – in the past couple of years – COVID-19, the leading causes of death today are chronic diseases . Heart disease has been the leading cause of death in the United States every year since 1921 with the exception of 2001 and 2002 when cancer and heart disease flip-flopped as the first and second cause of death, respectively. Until COVID-19 came on the scene and has since claimed the #3 spot, chronic lower respiratory disease – also referred to as chronic obstructive pulmonary disease (COPD) – was the 4th leading cause of death. COPD has been consistently a leading cause of death since the 1980’s. COPD is an umbrella term that includes conditions like emphysema, chronic bronchitis, pulmonary hypertension, and asthma. We will dive deeper into all of these conditions in later chapters.
Unintentional injuries have also been high on the list of leading causes of death in the United States over the past 100 years. Unintentional injuries include motor vehicle crashes, drownings, falls, burns, and poisonings/overdoses. The term “unintentional injuries” is the preferred term in public health over the term “accidents”, because “accidents” implies that the injury could not be prevented. You may recall the old saying “accidents happen”, suggesting that these injuries happen spontaneously and without avoidance. Through decades of scientific research, however, it has become evident that most of these unintentional injuries can be prevented, and public health initiatives have been implemented to prevent these injuries. For example, seat belt laws and cell phone use while driving laws have been passed to decrease motor vehicle crashes. Educational programs for parents to prevent childhood drownings and burns are offered through the CDC. Click here to read about these programs. Local agencies on aging offer fall prevention courses to community residents. Poison control centers throughout the country exist to prevent overdoses on everything from household chemicals to medication.
While unintentional injuries are the fourth leading cause of death in the United States for all ages, they are the leading cause of death in the United States for individuals 1-44 years of age. Therefore, individuals between 1-44 are most likely to die from an unintentional injury than any other cause. Of all of the types of unintentional injuries, motor vehicle crashes were the most common cause of unintentional death up until 2010. Then there was a significant shift and poisonings become the most common cause of unintentional death. This is directly associated with the opioid epidemic in the United States and the increased number of unintentional opioid overdoses. According to the CDC, 70% of the overdose deaths in 2019 involved an opioid.
Scan this QR code to access the table that outlines types of unintentional deaths since 1981.

Introduction to epidemiology
The traditional definition of epidemiology is the study of disease distribution and determinants. Throughout time, however, the definition has been broadened to include the array of health-related issues (e.g. opioid abuse), not just chronic and communicable diseases. The term “study” in the definition is important, because epidemiologists are scientists who use a systemized and data-driven approach to investigate diseases and other health issues.
The key measurements that are used to study diseases and other health issues and measure causes of death include mortality and morbidity rates, incidence rates, prevalence rates, attack rates, life expectancy, and years of potential life lost.
Morbidity rate – Morbidity is defined as any physiological or psychological condition that hinders a person’s wellbeing. Mortality rates are used to track the impact of these various conditions on a population.
Mortality rate – Mortality is synonymous with death. Mortality rates are used to measure the extent of life lost as a result of specified causes and conditions on a population.
Incidence, prevalence, and attack rates are the specific measurements used to study morbidity and mortality.
Incidence “is the occurrence of new cases of disease or injury in a population over a specified period of time.” https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section2.html Incidence rate is synonymous with and can also be referred to as attack rate.
Prevalence, “is the proportion of persons in a population who have a particular disease or attribute at a specified point in time or over a specified period of time. Prevalence differs from incidence in that prevalence includes all cases, both new and preexisting, in the population at the specified time, whereas incidence is limited to new cases only.”https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section2.html
This Epidemiologist’s Bathtub video uses the analogy of a bathtub to define incidence and prevalence rates
Life expectancy “tells us the average number of years of life a person who has attained a given age can expect to live. Life expectancy estimates from the National Center for Health Statistics provide a reliable snapshot of population health and mortality in the United States.”https://www.cdc.gov/nchs/nvss/life-expectancy.htm#publications. Life expectancies are calculated for various ages, from birth to over 100 years. The National Center for Health Statistics creates data tables and interactive maps that breakdown life expectancies by state and sex. Click here to access these tables.
Years of potential life lost (YPLL) – life expectancies are used as a benchmark on which YPLL are calculated. YPLL is a measure of premature death compared to average life expectancy. In the most general calculation, YPLL is the age of death subtracted from 75 (years of age). For example, if someone dies at 55, the YPLL is 75 – 55 = 20.
Epidemiologists are like doctors of an entire population. Whereas a primary care physician tracks their individual patients’ health history, an epidemiologist tracks the health history and patterns of an entire group of people, and depending on the health issue being studied, this group could be as small as a town or county in the case of a “food poisoning” outbreak or as large as the world in the case of a virus that has been transmitted across the globe.
Whether a local or global outbreak, an epidemiologist uses similar methods to investigate. They use descriptive and analytic studies to help determine who is more and less susceptible to being affected by the disease or other health-related issue. The aim of descriptive studies is to answer who, what, where, and when to generate hypotheses about a particular disease occurrence. Analytic studies are experimental or non-experimental studies designed to test hypotheses, ultimately aiming to determine the why and how about a particular disease occurrence. Watch this clip for more information about epidemiologists.
Theories of Disease Causation
A number of models of disease causation have been proposed to explore and attempt to explain how infectious and chronic diseases emerge. In Public Health it is important to understand how diseases develop to inform prevention efforts. This section introduces the three current models of disease causation: The Epidemiological Triad, the Chain of Infection, and the Multi-Causation Model. The first two are more often associated with explaining infectious disease causation and the third is associated with explaining chronic disease causation. Before diving deeper into these three models, however, it is important to define these terms: Endemic, epidemic, and pandemic. Endemic diseases commonly occur within a population at consistent rates that make them easier to track. Examples of endemic disease are the common cold, chicken pox in youth, and malaria in some regions of Africa. Epidemic diseases are unusual outbreaks or rates of a particular disease or health crisis in a specific population at a certain time. A classic example of an epidemic is the first Legionnaire’s outbreak in 1976 which affected attendees of the American Legion convention in Philadelphia, PA. The term epidemic also has been used to describe the obesity problem in the United States over the past two decades as well as the opioid crisis in more recent years. Considering the definition of an epidemic (exceptionally higher than average rates of a particular health issue affecting a certain population over a particular time period), this is an accurate use of the term. Obesity is an epidemic because its rates are confined to people living in the United States over the past 20 years. The “opioid epidemic” is also a correct use of the term for the same reason. Pandemic diseases are even wider-spreading than epidemics. A disease is considered a pandemic when it has spread across the globe. Examples of pandemics include COVID-19 and the 1918 Spanish influenza pandemics.
Epidemiological Triad
Among the simplest of these is the epidemiological triad or triangle, the traditional model for infectious disease. The triad consists of an external agent, a susceptible host, and an environment that brings the host and agent together. In this model, disease results from the interaction between the agent and the susceptible host in an environment that supports transmission of the agent from a source to that host. Two ways of depicting this model are shown in Figure 2.1. Notice in the figure the model on the left shows agent, host, and environment has having equal influence. The model on the right shows that the agent and host are variables that are dependent on each other with the environment.

Agent, host, and environmental factors interrelate in a variety of complex ways to produce disease. Different diseases require different balances and interactions of these three components. Development of appropriate, practical, and effective public health measures to control or prevent disease usually requires assessment of all three components and their interactions.
Agent originally referred to an infectious microorganism or pathogen: a virus, bacterium, parasite, or other microbe. Generally, the agent must be present for disease to occur; however, presence of that agent alone is not always sufficient to cause disease. A variety of factors influence whether exposure to an organism will result in disease, including the organism’s pathogenicity (ability to cause disease) and dose. There are five classes of agents that cause infectious disease: Bacteria, viruses, fungi, parasites, and prions. Bacteria and viruses cause most of the infectious diseases in the United States. Worldwide, however, parasites also contribute to a considerable number of infections, because malaria is caused by mosquitos which are classified as parasites.
Bacteria – Microscopic living organisms that are one-celled or multi-celled that are found virtually everywhere in our environment and even in our bodies. Bacteria can be healthy (such as the bacteria found in our colon), harmless, or can cause illness. Examples of bacterial infections include strep throat, staph infections, several types of pneumonia, and common sexually transmitted infections such as chlamydia and gonorrhea.
Viruses – Microscopic living organisms that borrow cell’s machinery to reproduce and burst out of cell or may stay in cell indefinitely without disturbing it very often do not present with symptoms. Someone may be infected with a virus, but not know it. Examples of viral infections include influenza, chickenpox, measles, hepatitis, and herpes.
Fungi – Fungi are multi-cellular organisms visible to the eye. Fungi are commonly occurring spores found essentially everywhere. About half of the fungi we encounter is harmless, some are even healthy. Internally, we have healthy fungi inside our colons and females have healthy vaginal fungi. The other half, however, can lead to infectious disease. Examples of fungal infections are various types of fungal rashes: Ringworm, athlete’s foot, jock itch, and nail fungus. All of these infections usually present with distinct and apparent signs. As a result, prognosis with these conditions is usually good, and treatment is relatively simple. Internal fungal infections, such as fungal pneumonia (i.e. Coccidioidomycosis) which is transmitted from exposure to contaminated soil, are more likely to be asymptomatic or present with more general symptoms that mimic other less severe conditions (e.g. common cold, allergies) and may not get properly treated right away leading to more serious issues.
Parasites – these infectious agents range from microscopic one-celled protozoa to larger organisms classified as helminths (e.g. tapeworms, pinworms) and ectoparasites (e.g. ticks, lice). Depending on the type, some parasites can multiply in humans causing sickness. Others, like mosquitos, serve as arthropod vectors which cause disease themselves and also carry the disease from person to person. Parasitic infections are typically endemic in the United States, but malaria (a parasitic infection caused by mosquitos) is responsible for a substantial burden worldwide.
Prions – infectious agents that cause very rare and always fatal neurodegenerative changes to the brain. The two primary diseases are Creutzfeldt-Jakob disease (CJD) and kuru. Most CJD cases are random. It is not transmitted via person-to-person contact or through environmental contamination. A small percentage of cases are caused by an inherited gene mutation. CJD is ultimately fatal, with most people dying within a year of onset. Kuru also is a rare and always fatal neurodegenerative disease that is most often linked to consuming infected brain tissue. Kuru was most notably transmitted among the people of New Guinea who would eat the brains of their deceased as part of a funeral ritual. Similar to CJD, most people die within one year of onset of symptoms.
Over time, the concept of agent has been broadened to include chemical and physical causes of disease or injury. These include chemical contaminants (such as the L-tryptophan contaminant responsible for eosinophilia-myalgia syndrome), as well as physical forces (such as repetitive mechanical forces associated with carpal tunnel syndrome). While the epidemiological triad serves as a useful model for many diseases, it has proven inadequate for cardiovascular disease, cancer, and other diseases that appear to have multiple contributing causes without a single necessary one.
Host refers to the human who can get the disease. A variety of factors intrinsic to the host, sometimes called risk factors, can influence an individual’s exposure, susceptibility, or response to a causative agent. Opportunities for exposure are often influenced by behaviors such as sexual practices, hygiene, and other personal choices as well as by age and sex. Susceptibility and response to an agent are influenced by factors such as genetic composition, nutritional and immunologic status, anatomic structure, presence of disease or medications, and psychological makeup.
Environment refers to extrinsic factors that affect the agent and the opportunity for exposure. Environmental factors include physical factors such as geology and climate, biologic factors such as insects that transmit the agent, and socioeconomic factors such as crowding, sanitation, and the availability of health services.
CDC, 2012, paras. 1-12.
Chain of Infection
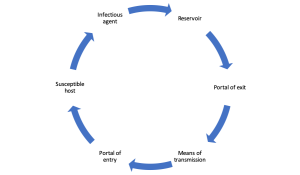
As described above, the traditional epidemiologic triad model illustrates that infectious diseases result from the interaction of agent, host, and environment. The chain of infection model looks at the transmission of infectious disease more specifically. There are six chains in the chain of infection: Infectious agent, reservoir, portal of exit, means of transmission, portal of entry, and susceptible host. The infectious agent leaves its reservoir or host through a portal of exit, by a means of transmission, and enters through an appropriate portal of entry to infect a susceptible host. The infectious agent is any of the five types of infectious agents discussed earlier in the chapter (i.e. bacteria, viruses, fungi, parasites, and prion). The reservoir can be a human or other animal, soil, or water and serves as the host for the infectious agent, providing it with an environment in which the agent can thrive. Portals of exit are how the agent can leave the reservoir. In humans, for example, portals of exit include respiratory secretions, feces, blood, semen, vaginal secretions, breast milk, open sores, and conjunctiva of the eyes. Portals of entry are the same as portals of exit. Portals serve as exit portals if the infection is leaving the infected host, and serve as entry portals if the infection is entering a new host. In other words, the infectious agent leaves the infected host via their portal of exit and enters the new host via their portal of entry. The means of transmission is how the agent goes from portal of exit to portal of entry. Examples of means of transmission include direct contact (e.g. kissing), indirect contact (e.g. a person sneezes on another person), a vector (e.g. a mosquito bite), and a vehicle (e.g. eating contaminated food). The susceptible host is the potential new reservoir for the infectious agent to thrive. Factors that increase susceptibility include having a compromised immune system, having diabetes or another chronic disease, recently undergoing surgery, having HIV/AIDS, not being vaccinated against that particular infection, and age (infants and seniors are more susceptible). Figure 2.2 illustrates the cyclical order of the chain of infection.
Reservoir
The reservoir of an infectious agent is the habitat in which the agent normally lives, grows, and multiplies. Reservoirs include humans, animals, and the environment. The reservoir may or may not be the source from which an agent is transferred to a host. For example, the reservoir of Clostridium botulinum is soil, but the source of most botulism infections is improperly canned food containing C. botulinum spores.
Human reservoirs. Many common infectious diseases have human reservoirs. Diseases that are transmitted from person to person without intermediaries include the sexually transmitted infections (STI), measles, mumps, streptococcal infection, and many respiratory pathogens. Because humans were the only reservoir for the smallpox virus, naturally occurring smallpox was eradicated after the last human case was identified and isolated.
Human reservoirs may or may not show the effects of illness. Asymptomatic or passive or healthy carriers are those who never experience symptoms despite being infected. Incubatory carriers are those who can transmit the agent during the incubation period before clinical illness begins. Convalescent carriers are those who have recovered from their illness but remain capable of transmitting to others. Chronic carriers are those who continue to harbor a pathogen such as hepatitis B virus or Salmonella Typhi, the causative agent of typhoid fever, for months or even years after their initial infection. One notorious carrier is Mary Mallon, or Typhoid Mary, who was an asymptomatic chronic carrier of Salmonella Typhi. As a cook in New York City and New Jersey in the early 1900s, she unintentionally infected dozens of people until she was placed in isolation on an island in the East River, where she died 23 years later.
Carriers commonly transmit disease because they do not realize they are infected, and consequently take no special precautions to prevent transmission. Symptomatic persons who are aware of their illness, on the other hand, may be less likely to transmit infection because they are either too sick to be out and about, take precautions to reduce transmission, or receive treatment that limits the disease.
Animal reservoirs. Humans are also subject to diseases that have animal reservoirs. Many of these diseases are transmitted from animal to animal, with humans as incidental hosts. The term zoonosis refers to an infectious disease that is transmissible under natural conditions from vertebrate animals to humans. Long recognized zoonotic diseases include brucellosis (cows and pigs), anthrax (sheep), plague (rodents), trichinellosis/trichinosis (swine), tularemia (rabbits), and rabies (bats, raccoons, dogs, and other mammals). Zoonoses newly emergent in North America include West Nile encephalitis (birds), and monkeypox (prairie dogs). Many newly recognized infectious diseases in humans, including HIV/AIDS, Ebola infection and SARS, are thought to have emerged from animal hosts, although those hosts have not yet been identified.
Environmental reservoirs. Plants, soil, and water in the environment are also reservoirs for some infectious agents. Many fungal agents, such as those that cause histoplasmosis, live and multiply in the soil. Outbreaks of Legionnaires disease are often traced to water supplies in cooling towers and evaporative condensers, reservoirs for the causative organism Legionella pneumophila.
Portal of exit
Portal of exit is the path by which a pathogen leaves its host. The portal of exit usually corresponds to the site where the pathogen is localized. For example, influenza viruses and Mycobacterium tuberculosis exit the respiratory tract, schistosomes through urine, cholera vibrios in feces, Sarcoptes scabiei in scabies skin lesions, and enterovirus 70, a cause of hemorrhagic conjunctivitis, in conjunctival secretions. Some bloodborne agents can exit by crossing the placenta from mother to fetus (rubella, syphilis, toxoplasmosis), while others exit through cuts or needles in the skin (hepatitis B) or blood-sucking arthropods (malaria).
Modes of transmission
An infectious agent may be transmitted from its natural reservoir to a susceptible host in different ways. There are different classifications for modes of transmission. Here is one classification:
- Direct
- Direct contact
- Droplet spread
- Indirect
- Airborne
- Vehicle-borne
- Vector-borne (mechanical or biologic)
In direct transmission, an infectious agent is transferred from a reservoir to a susceptible host by direct contact or droplet spread.
Direct contact occurs through skin-to-skin contact, kissing, and sexual intercourse. Direct contact also refers to contact with soil or vegetation harboring infectious organisms. Thus, infectious mononucleosis (“kissing disease”) and gonorrhea are spread from person to person by direct contact. Hookworm is spread by direct contact with contaminated soil.
Droplet spread refers to spray with relatively large, short-range aerosols produced by sneezing, coughing, or even talking. Droplet spread is classified as direct because transmission is by direct spray over a few feet, before the droplets fall to the ground. Pertussis and meningococcal infection are examples of diseases transmitted from an infectious patient to a susceptible host by droplet spread.
Indirect transmission refers to the transfer of an infectious agent from a reservoir to a host by suspended air particles, inanimate objects (vehicles), or animate intermediaries (vectors).
Airborne transmission occurs when infectious agents are carried by dust or droplet nuclei suspended in air. Airborne dust includes material that has settled on surfaces and become resuspended by air currents as well as infectious particles blown from the soil by the wind. Droplet nuclei are dried residue of less than 5 microns in size. In contrast to droplets that fall to the ground within a few feet, droplet nuclei may remain suspended in the air for long periods of time and may be blown over great distances. Measles, for example, has occurred in children who came into a physician’s office after a child with measles had left, because the measles virus remained suspended in the air.
Vehicles that may indirectly transmit an infectious agent include food, water, biologic products (blood), and fomites (inanimate objects such as handkerchiefs, bedding, or surgical scalpels). A vehicle may passively carry a pathogen — as food or water may carry hepatitis A virus. Alternatively, the vehicle may provide an environment in which the agent grows, multiplies, or produces toxin — as improperly canned foods provide an environment that supports production of botulinum toxin by Clostridium botulinum.
Vectors such as mosquitoes, fleas, and ticks may carry an infectious agent through purely mechanical means or may support growth or changes in the agent. Examples of mechanical transmission are flies carrying Shigella on their appendages and fleas carrying Yersinia pestis, the causative agent of plague, in their gut. In contrast, in biologic transmission, the causative agent of malaria or guinea worm disease undergoes maturation in an intermediate host before it can be transmitted to humans.
Portal of entry
The portal of entry refers to the manner in which a pathogen enters a susceptible host. The portal of entry must provide access to tissues in which the pathogen can multiply or a toxin can act. Often, infectious agents use the same portal to enter a new host that they used to exit the source host. For example, influenza virus exits the respiratory tract of the source host and enters the respiratory tract of the new host. In contrast, many pathogens that cause gastroenteritis follow a so-called “fecal-oral” route because they exit the source host in feces, are carried on inadequately washed hands to a vehicle such as food, water, or utensil, and enter a new host through the mouth. Other portals of entry include the skin (hookworm), mucous membranes (syphilis), and blood (hepatitis B, human immunodeficiency virus).
Host
The final link in the chain of infection is a susceptible host. Susceptibility of a host depends on genetic or constitutional factors, specific immunity, and nonspecific factors that affect an individual’s ability to resist infection. An individual’s genetic makeup may either increase or decrease susceptibility. For example, persons with sickle cell trait seem to be at least partially protected from a particular type of malaria. Specific immunity refers to protective antibodies that are directed against a specific agent. Such antibodies may develop in response to infection, vaccine, or toxoid (toxin that has been deactivated but retains its capacity to stimulate production of toxin antibodies) or may be acquired by transplacental transfer from mother to fetus or by injection of antitoxin or immune globulin. Nonspecific factors that defend against infection include the skin, mucous membranes, gastric acidity, cilia in the respiratory tract, the cough reflex, and nonspecific immune response. Factors that may increase susceptibility to infection by disrupting host defenses include malnutrition, alcoholism, and disease or therapy that impairs the nonspecific immune response.
Implications for public health
The goal is to break the chain of infection as early as possible. Most chains cannot be broken at the infectious agent link, because infectious agents naturally occur in the environment. Therefore, we must target breaking the chain at the reservoir level or later. Examples of breaking the chain at the reservoir link include properly storing and cooking raw meat and poultry, eliminating standing water that could attract mosquitos, and quarantining if you have an infection that can be passed to others. Examples of breaking the chain at the portal of exit link include wearing a mask if you have an infection that could be passed to others, wearing a condom to prevent passing an STI, and covering an infected sore. Breaking the chain at the means of transmission link includes washing your hands, covering your mouth and nose when you sneeze, and disinfecting surfaces. Breaking the chain at the portal of entry link includes wearing personal protective equipment (PPE) to prevent getting an infection passed onto you, putting a bandage on a fresh wound to prevent it from getting infected, and wearing a condom to prevent getting an STI. Hosts can be less susceptible by staying current on their vaccinations, properly managing their chronic conditions, and maintaining a healthy diet. Figure 2.3 illustrates an example of how the chain of infection works in the case of the common cold.
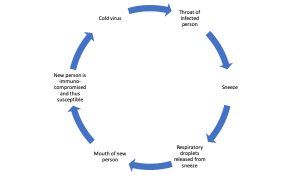
In the above illustration of an example of the perpetuation of the chain of infection, a pathogen (cold virus), leaves reservoir (throat of infected person), when host sneezes (portal of exit-nose and mouth). Means of transmission (saliva droplets) enter respiratory tract of susceptible host at close range (portal of entry-mouth). New infection possibly established. If one link is missing, chain is broken. This clip further explains the chain of infection.
Knowledge of the portals of exit and entry and modes of transmission provides a basis for determining appropriate control measures. In general, control measures are usually directed against the segment in the infection chain that is most susceptible to intervention, unless practical issues dictate otherwise.
Interventions are directed at controlling or eliminating agent at source of transmission, protecting portals of entry, and increasing the host’s defenses. For some diseases, the most appropriate intervention may be directed at controlling or eliminating the agent at its source. A patient sick with an infectious disease may be treated with antibiotics to eliminate the infection. An asymptomatic but infected person may be treated both to clear the infection and to reduce the risk of transmission to others. In the community, soil may be decontaminated or covered to prevent escape of the agent.
Some interventions are directed at the mode of transmission. Interruption of direct transmission may be accomplished by isolation of someone with infection, or counseling persons to avoid the specific type of contact associated with transmission. Vehicle-borne transmission may be interrupted by elimination or decontamination of the vehicle. To prevent fecal-oral transmission, efforts often focus on rearranging the environment to reduce the risk of contamination in the future and on changing behaviors, such as promoting handwashing. For airborne diseases, strategies may be directed at modifying ventilation or air pressure, and filtering or treating the air. To interrupt vector-borne transmission, measures may be directed toward controlling the vector population, such as spraying to reduce the mosquito population.
Some strategies that protect portals of entry are simple and effective. For example, bed nets are used to protect sleeping persons from being bitten by mosquitoes that may transmit malaria. A dentist’s mask and gloves are intended to protect the dentist from a patient’s blood, secretions, and droplets, as well to protect the patient from the dentist. Wearing of long pants and sleeves and use of insect repellent are recommended to reduce the risk of Lyme disease and West Nile virus infection, which are transmitted by the bite of ticks and mosquitoes, respectively.
Some interventions aim to increase a host’s defenses. Vaccinations promote development of specific antibodies that protect against infection. On the other hand, prophylactic use of antimalarial drugs, recommended for visitors to malaria-endemic areas, does not prevent exposure through mosquito bites, but does prevent infection from taking root.
Finally, some interventions attempt to prevent a pathogen from encountering a susceptible host. The concept of herd immunity suggests that if a high enough proportion of individuals in a population are resistant to an agent, then those few who are susceptible will be protected by the resistant majority, since the pathogen will be unlikely to “find” those few susceptible individuals. The degree of herd immunity necessary to prevent or interrupt an outbreak varies by disease. In theory, herd immunity means that not everyone in a community needs to be resistant (immune) to prevent disease spread and occurrence of an outbreak. In practice, herd immunity has not prevented outbreaks of measles and rubella in populations with immunization levels as high as 85% to 90%. One problem is that, in highly immunized populations, the relatively few susceptible persons are often clustered in subgroups defined by socioeconomic or cultural factors. If the pathogen is introduced into one of these subgroups, an outbreak may occur,” (CDC, 2012, paras. 1-23).
Check for Understanding :Click on the link that is broken in this scenario
Multi-Causation Model
As illustrated with the epidemiological triad and chain of infection, causes of infectious disease are more finite. After all, there are only five types of infectious agents. Analyzing and determining causes of chronic diseases is more complex, because the causes of chronic disease are multi-faceted. The multi-causation model is more appropriate to use when delineating possible causes of chronic disease. Figure 2.4 illustrates the multi-causation model.
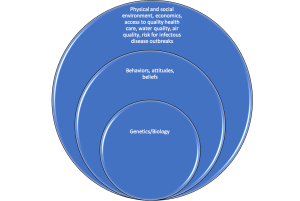
The above image illustrates the multi-causation model. In the center of the model is the individual (aka host) and their genetic makeup. In public health we consider this genetic endowment un-modifiable and therefore not the target for health interventions. Moving outward from the individual, however, are intrapersonal and interpersonal factors such as attitudes, beliefs, values, and behavioral choices. These factors are followed by societal and organizational factors such as environment, economics, and healthcare. These levels are common targets for public health interventions, because they are considered modifiable.
Genetics and biology consist of the DNA passed down from biological parents. It also includes anatomy and physiology and chemical makeup. For the most part, these factors cannot be changed once a person is born. In public health, this level is not often the focus for prevention or protection interventions.
Intrapersonal and interpersonal factors, however, are used to analyze risk for infectious and chronic disease, and therefore often the foci of health interventions. For example, the belief that condom use dulls sensation during intercourse may result in low condom use rates and therefore increasing the risk for STI transmission. One’s risk for several chronic diseases (cancer, stroke, heart disease, COPD) is increased with the behavioral choice to smoke cigarettes or vape.
The outer-most layer includes the social determinants of health (SDOH). SDOH “are conditions in the places where people live, learn, work, and play that affect a wide range of health and quality-of life-risks and outcomes” (CDC, 2021, para. 1). These include exposure to physical and chemical environmental toxins (e.g., air, soil, and water pollution), climate, possible exposure to infectious agents, and access to healthcare. Different climates post different health risks. For example, living in a tropical climate like Central America poses more risk for Dengue Fever transmitted by mosquitos that thrive in this climate. Limited access to healthcare has been shown to have significant impact on one’s risk for disease. For example, uninsured American adults are less likely to receive preventative care and are therefore at a higher risk for the leading chronic diseases in the United States. Further, access to quality healthcare is equally important. Not all health care is quality healthcare. Research has shown that quality healthcare resources are more prevalent in communities in which a high number of the population has health insurance, whereas lower-income and rural areas may be more prone to physician shortage, resulting in limited opportunities for appointments and longer wait times.
Risk Factors and Protective Factors for Disease
A person’s likelihood of getting a disease is often explained by analyzing their risk and protective factors for that disease. “Risk factors are characteristics at the biological, psychological, family, community, or cultural level that precede and are associated with a higher likelihood of negative outcomes,” (SAMHSA, n.d., para. 3). “Protective factors are characteristics associated with a lower likelihood of negative outcomes or that reduce a risk factor’s impact. Protective factors may be seen as positive countering events,” (SAMHSA, n.d., para, 4).
According to the National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), six in ten adults living in the United States have a chronic disease and four in ten adults living in the United States have two or more chronic diseases. The latter statistic brings up the term co-morbidity. Co-morbidity is when a person has been diagnosed with two or more diseases. You likely can think of at least one person in your life who has co-morbidities. Maybe somebody has arthritis and asthma. Both of those are chronic conditions. Maybe it’s cancer and diabetes. Again, both chronic conditions. Co-morbidities are so frequent because many of the most commonly diagnosed chronic diseases have shared risk factors . In fact, the NCCDPHP identifies four risk factors that contribute to most chronic diseases:
1). Tobacco use or exposure to secondhand smoke
2). Poor nutrition
3). Lack of physical activity
4). Excessive alcohol use
These four risk factors are linked to heart disease, cancer, stroke, COPD, unintentional injuries, diabetes, Alzheimer’s disease, and chronic kidney disease. Understanding the magnitude of overlap among these risk factors and disease informs health program development. For example, participating in an effective nutrition program can lessen one’s risk for most of these chronic diseases, because poor nutrition is a risk factor for the majority of them.
Preventing the Burden of Disease
Most infectious and chronic diseases can be prevented to some extent, either preventing disease from its inception or preventing the disease from worsening with the right diagnosis and intervention. There are three levels of prevention: Primary, secondary, and tertiary. Primary prevention means avoiding the disease altogether. Examples of primary prevention include eating a healthy diet; exercising regularly; avoiding alcohol, tobacco, and other drug use; getting adequate sleep; managing stress in healthy ways; getting vaccinated; and maintaining proper oral hygiene. Engaging in these healthy behaviors reduces the risk of disease occurrence. Secondary prevention means catching the disease soon after onset, thereby reducing the severity. Examples include screenings of all kinds (e.g. cancer screenings, blood pressure screenings), modified diets to manage pre-diabetes, and contact tracing of infectious disease. True prevention is aimed at the primary and secondary levels. Public health interventions target these two levels. Tertiary prevention is synonymous with rehabilitation, and involves measures to get a person back to their state of health prior to the onset of signs and symptoms and to lessen the chance of subsequent burdens of disease. Examples include cardiac and stroke rehabilitation, cancer treatment (e.g. chemotherapy, radiation), and chronic disease management programs.
Healthy People 2030
Healthy People is the framework for addressing the nation’s health. Healthy People 2030 includes 355 core objectives that span the gamut of health issues affecting people living in the United States. In addition to these measurable objectives, the framework includes Leading Health Indicators (LHI) which are a sub-set of high-priority objectives that address the most significant factors contributing to disease risk and occurrence. There are approximately 23 LHI that are categorized by life span/age. Click here to read through the LHI’s.
Recall quiz
Chain of Infection Recall Quiz
Discussion Questions
- List all of the LHI’s that are related to infectious and chronic disease.
- Link the four most common risk factors to chronic disease with the current leading causes of death. Which risk factors are associated with these leading causes of death?
- Apply the MCM of disease to heart disease. Be sure to include all of the social determinants.
- Refer to the table that lists the leading causes of death between 1900 and today, and discuss similarities and differences. What contributes to these deaths? What are risk factors? What are protective factors?
Chapter Activity
1). Read the Anthrax fact sheet and answer the questions in Exercise 1.8 found here https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section8.html
references
Adams, D. P. (2021). Foundations of Infectious Disease: A Public Health Perspective. Jones & Bartlett.
Anderson, R. N., & Smith, B. L. (2003). Deaths: leading causes for 2001. National vital statistics reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 52(9), p. 1–85.
Baylor College of Medicine. (n.d.). Introduction to infectious diseases. Retrieved September 29, 2022, from https://www.bcm.edu/departments/molecular-virology-and-microbiology/emerging-infections-and-biodefense/introduction-to-infectious-diseases#:~:text=The%20majority%20of%20agents%20that
Centers for Disease Control and Prevention. (1900). Leading causes of death, 1900-1998. https://www.cdc.gov/nchs/data/dvs/lead1900_98.pdf
Centers for Disease Control and Prevention. (2012). Fungal pneumonia: a silent epidemic Coccidioidomycosis (valley fever). https://www.cdc.gov/fungal/pdf/cocci-fact-sheet-sw-us-508c.pdf
Centers for Disease Control and Prevention. (2013). Descriptive and analytic studies [PowerPoint]. https://www.cdc.gov/globalhealth/healthprotection/fetp/training_modules/19/desc-and-analytic-studies_ppt_final_09252013.pdf
Centers for Disease Control and Prevention. (2016, June 17). What is epidemiology? https://www.cdc.gov/careerpaths/k12teacherroadmap/epidemiology.html
Centers for Disease Control and Prevention. (2019a). Creutzfeldt-Jakob Disease, Classic (CJD). https://www.cdc.gov/prions/cjd/index.html
Centers for Disease Control and Prevention. (2019b). Parasites. https://www.cdc.gov/parasites/about.html
Centers for Disease Control and Prevention. (2020a). Dengue around the world. https://www.cdc.gov/dengue/areaswithrisk/around-the-world.html
Centers for Disease Control and Prevention. (2020b). Principles of epidemiology. https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section8.html
Centers for Disease Control and Prevention. (2020c, July 10). Injury prevention & control. Www.cdc.gov. https://www.cdc.gov/injury/wisqars/animated-leading-causes.html
Centers for Disease Control and Prevention. (2020d, October 23). Social determinants of health. https://www.cdc.gov/publichealthgateway/sdoh/index.html
Centers for Disease Control and Prevention. (2021a, April 28). About chronic diseases. https://www.cdc.gov/chronicdisease/about/index.htm
Centers for Disease Control and Prevention. (2021b, June 16). Drowning prevention. https://www.cdc.gov/drowning/prevention/index.html
Centers for Disease Control and Prevention. (2021c, June 23). Drug overdose deaths. https://www.cdc.gov/drugoverdose/deaths/index.html
Centers for Disease Control and Prevention. (2022). Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
Cleveland Clinic. (2020). Skin fungus. https://my.clevelandclinic.org/health/diseases/4276-skin-fungus
Hamann, B. (2007). Disease: Identification, Prevention, and Control (3rd ed.). McGraw-Hill Higher Education.
Leavitt, J. (1996). Typhoid Mary: Captive to the Public’s Health. Beacon Press.
Office of Disease Prevention and Health Promotion. (2020). Healthy People 2030. Health.gov. https://health.gov/healthypeople.
Remington, P. L., Hall, W. N., Davis, I. H., Herald, A., & Gunn, R. A. (1985). Airborne transmission of measles in a physician’s office. JAMA, 253(11), 1574–1577.
Seabert, D., & Mckenzie, J. F. (2022). An Introduction to Community & Public Health. Jones & Bartlett Learning.
Substance Abuse and Mental Health Services Administration. (2019). Risk and protective factors. https://www.samhsa.gov/sites/default/files/20190718-samhsa-risk-protective-factors.pdf
Conditions caused by organisms, such as bacteria or viruses that are transmitted via humans; animals or insects; or contaminated food, water, or soil.
A disease or condition with a sudden onset. Many can be severe. Most acute diseases last fewer than three months.
Non-contagious diseases that typically come on slowly and last more than three months. Many will last a person's lifetime.
Risk factors for a disease that cannot be changed.
Risk factors for a disease that have the ability to be changed through individual or community intervention.