9 Chapter 9: Cardiovascular and Cerebrovascular Disease
Brandye Nobiling
Chapter Objectives:
- Identify signs, symptoms, risks, treatment, and prevention of various types of cardiovascular disease and stroke
- Discern among blood pressure readings
- Discuss how social determinants of health are associated with risk for cardiovascular disease and stroke
- Describe current public health interventions aimed at improving cardio and cerebrovascular health in in the US
INTRODUCTION
Cardiovascular and cerebrovascular diseases refer to conditions that affect the following parts of the body:
- Cardio = heart
- Cerebro = brain
- Vascular = blood vessels
Cardiovascular diseases include heart attacks, heart failure, atherosclerosis, arrhythmias, and heart valve problems (e.g., heart murmur). Cerebrovascular disease is synonymous with stroke. Hypertension (aka high blood pressure) is also included in this chapter as it is a risk factor for other cardiovascular and cerebrovascular conditions. “Cardiovascular disease is the broad term for problems with the heart and blood vessels. These problems are often due to atherosclerosis. This condition occurs when fat and cholesterol build up in blood vessel (artery) walls. This buildup is called plaque. Over time, plaque can narrow blood vessels and cause problems throughout the body. If an artery becomes blocked, it can lead to heart attack or stroke,” (U.S. National Library of Medicine, 2022, para 1).
“More than 120 million Americans have been diagnosed with some form of cardiovascular disease, including coronary heart disease (CHD), hypertension, heart failure, and stroke. By 2035, more than 130 million adults are projected to have some form of cardiovascular disease, and health care costs are expected to exceed $1 trillion” (Baptiste, D. et al., 2021, p. 41). Therefore, cardiovascular and cerebrovascular diseases are serious public health concerns.
Check for Understanding: Blood flow
Hypertension
Hypertension (also called high blood pressure or HBP) “is an established risk factor for cardiovascular disease (CVD) and contributes to 1 in 7 cardiovascular-related deaths” (Commodore-Mensah, et al., 2021, p. 707). Hypertension is referred to as the silent killer, because most of the time there are no signs and symptoms, and it can be a precursor to heart attack, heart failure, and stroke. The only way to know if you have HBP is by regularly getting your blood pressure checked and learning about your blood pressure readings.
A blood pressure reading is a series of two numbers. The first number (top number) is the systolic blood pressure, which is defined as the push of blood flow when the heart is contracting (beating). The second number (bottom number) is the diastolic blood pressure, which is the push of blood flow when the heart is relaxed between beats. The systolic pressure is a higher number than the diastolic because there is higher pressure when the heart is beating compared to when the heart is resting between beats.
What is normal blood pressure? Is 120/80 “good”? Not anymore. According to the American Heart Association, healthy blood pressure is under 120/80 (but not below 90/60 which is considered low blood pressure or hypotension). From there, levels are categorized according to the chart in Figure 9.1. Click here to read more about what blood pressure readings mean: https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings
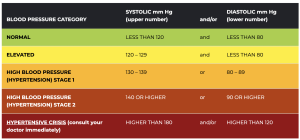
A diagnosis of hypertension will require multiple high readings. From there, a healthcare provider may recommend purchasing an at-home blood pressure monitor and/or prescribe medication to lower and manage hypertension. There are numerous medications that may be taken to reduce the workload of the heart and allow blood to move easier throughout the blood vessels. Click here to learn more about these medications: https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
Prevention of Hypertension
There are two types of hypertension, essential (also called primary) and secondary. Secondary hypertension is caused by one direct and known condition (e.g., kidney disease, pregnancy, taking certain medications). Essential hypertension, however, is high blood pressure not caused by another medical condition. Public Health professionals are focused on primary and secondary prevention of essential hypertension, and those efforts start with knowing common risk factors for essential hypertension. These risk factors include:
- Having a sedentary lifestyle/limited physical activity
- Being obese
- Consuming an excessive amount of alcohol or caffeinated beverages
- Consuming a diet high in salt and unhealthy fat
- Having a family history of hypertension
- Being an older adult (65 years and older)
- Having sleep issues
- Smoking
The good news is that most of these risk factors are modifiable. Click on each of the links in the table below to read about some individual strategies to manage these modifiable risk factors for hypertension.
Table 9.1 Risk Factors for CV Disease
Atherosclerosis
Atherosclerosis is a type of arteriosclerosis in which a fatty plaque builds up in the arteries. This build-up restricts the flow of blood, oxygen, and nutrients throughout the body. Initially this is an asymptomatic process, and some individuals suffering from atherosclerosis may not know they have the condition until it results in a heart attack or stroke. Blockages in arteries supplying the heart may lead to a heart attack, and blockages in arteries supplying the brain may lead to a stroke.
Click here to learn about signs/symptoms, complications, risk factors, treatment, and prevention for atherosclerosis:
Coronary Artery Disease (CAD)
“Coronary artery disease (CAD) is the most common type of heart disease in the United States. It is sometimes called coronary heart disease or ischemic heart disease,” (CDC, 2021, para 1). CAD is caused by atherosclerosis affecting one or more arteries that supply the heart. Like atherosclerosis, CAD may be asymptomatic and can lead to a heart attack.
Click here to learn about signs/symptoms, complications, risk factors, treatment, and prevention for CAD.
Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) is a common condition that occurs when atherosclerotic plaque builds up in the arteries that supply the arms or legs. Click here to learn about signs/symptoms, complications, risk factors, treatment, and prevention for PAD.
Congestive Heart Failure (CHF)
“Heart failure, or congestive heart failure, is a long-term condition that gets worse over time. Although the name sounds like your heart has stopped working, heart failure means your heart isn’t able to pump blood as well as it should. When your heart has less pumping power, that can damage your organs and fluid can collect in your lungs,” (Cleveland Clinic, 2021, para 2).
Click here to learn about signs/symptoms, complications, risk factors, treatment, and prevention for CHF.
Heart Attack
“A heart attack, also called a myocardial infarction, happens when a part of the heart muscle doesn’t get enough blood. The more time that passes without treatment to restore blood flow, the greater the damage to the heart muscle. CAD is the most common cause of a heart attack,” (CDC, 2022, para 2).
Signs and symptoms differ between biological sexes. You will notice in Figure 9.2 that the “classic” symptoms of a heart attack are more common in men, while women tend to have different symptoms of a heart attack. This overlook in scientific research is one of the reasons women have been suffering heart attacks in silence historically. Luckily more research now is exploring CAD in women, including signs/symptoms, risk factors, and prevention of CAD.

Arrhythmias
Cardiac arrhythmias result from an interference with the heart’s electrical conduction system. As a result, the heart may beat too fast (tachycardia), too slow (bradycardia), or have an abnormal rhythm (atrial fibrillation, ventricular fibrillation, heart block). The following links provide additional information on each type of arrhythmia:
- Click here to view animations of each type of arrhythmia.
- Click here to learn about tachycardia.
- Click here to learn about bradycardia.
- Click here to learn about atrial fibrillation.
- Click here to learn about ventricular fibrillation.
- Click here to learn about prevention and treatment for arrhythmias.
Stroke
Stroke is the fifth leading cause of death and the leading cause of disability in the United States. There are two types of stroke, an ischemic stroke and a hemorrhage stroke. An ischemic stroke is caused by a blood clot restricting blood flow to the brain. A hemorrhagic stroke is caused by a ruptured blood vessel that restricts blood flow to the brain. The effects of stroke are determined what part(s) of the brain were damaged. Click here to learn what results from damage to the left and right side of the cerebral cortex. Click here to learn what happens when a stroke affects the brainstem.
Watch this video for an overview of stroke.
A transient ischemic attack (TIA) is a “warning stroke” during which a blood clot temporarily restricts blood flow to the brain. Effects of a TIA are not severe like an actual stroke because blood flow was only restricted temporarily. But, TIA’s are a leading risk factor for stroke. If someone has a TIA they should seek medical care to prevent having a future stroke.
A key to surviving a stroke is to know common signs and symptoms. The acronym F.A.S.T. is used to outline stroke symptoms:
F = face drooping on one side
A = arm weakness or numbness on one side of the body
S = speech slurring or difficulty talking
T = time to call 911
In addition to the these symptoms, people having a stroke may have dizziness or trouble walking, vision problems in one eye, and confusion. It needs to be underscored that symptoms of a stroke come on suddenly and only one side of the body is affected.
Stroke is a life-altering event, and rehabilitation is needed after someone survives a stroke. Occupational and physical therapy help restore abilities to pre-stroke levels as much as possible. Mental health counseling is an important part of rehabilitation as stroke victims are vulnerable to depression and anxiety. It is a long journey and it is important to celebrate the little victories along the way. The American Stroke Association has created a “life after stroke” workbook to help stroke patients navigate their “new normal”. Read it here.
Social Determinants and Cardio and Cerebrovascular Disease
As stated in Chapter 2, cardiovascular disease is the leading cause of death and stroke is the fifth leading cause of death in the United States. Since the identification of risk factors in the 1900’s many efforts have gone into modifying individual risk factors, such as diet, physical activity, tobacco use, alcohol consumption, and stress. Commonly, these efforts are focused on primary and secondary prevention of CVD through interventions that target individuals as opposed to whole populations. Programs targeting smoking cessation, increased physical activity, better nutrition, and stress management have been successful in making general improvements in heart health. But, “despite advances in the primary and secondary prevention of CVD, there are still gross inequalities in cardiovascular health care across space and time” (Kreatsoulas, C & Sonia, S.A., 2010, p. 8C). These inequities are linked to all social determinants. A well-documented inverse association is between education level and CVD morbidity and mortality, meaning as education level increases, risk for CVD morbidity and mortality decrease. Another area of concern is access to quality health care, in particular insurance status (i.e. whether or not someone has health insurance). “The expansion of health insurance access with the Affordable Care Act demonstrated that expanded insurance coverage for low-income populations was associated with greater health care utilization, including improved access to primary and subspecialty care as well as increased access to prescription drugs,” (Powell-Wiley, T.M., et al., 2022, p. 789).
A third area of concern is race and ethnicity. According to the American Heart Association, declines in CVD mortality have not eliminated racial and ethnic differences in CVD; they remain constant,” (Havranek, E.P., 2015, p. 876). Health inequities among racial and minority groups are rooted in social determinants as opposed to biological factors. Findings from the wealth of research on health disparities indicate systemic racism and health care provider bias contribute to higher CVD morbidity and mortality among black and Hispanic populations. Some research findings indicate structural racism is the root determinant that impacts other social determinants, such as neighborhood and food environment. Researchers have shown inverse associations between access to food sources and health indicators (including CVD morbidity/mortality), meaning the more access to quality food sources the lower the CVD morbidity and mortality rates in a population. Longitudinal studies have shown that black and Hispanic/Latin X populations are most affected by this association, implying lack of quality food availability in neighborhoods that are primarily black and Hispanic/Latin X. In addition to social determinants impacting eating patterns based on the availability of healthy food options, social determinants are also linked to other individual risk behaviors of substance use, obesity, lack of physical activity, and stress management.
In addition to CVD, studies have linked the same social determinants to stroke morbidity and mortality. For example, in one study, researchers used the CDC’s Interactive Atlas of Heart Disease and Stroke to explore stroke mortality and hospitalizations among counties in the United States. Researchers found that hospitalizations for stroke here higher among those with no college degree, no park access (implying neighborhood and built environment), female head of household (implying single income household), on Medicare (implying medical care access and lower income level), and on food assistance (implying low income), (Yadav, R.S., 2022).
Public Health Efforts
To reach the overarching goal of eliminating health disparities, Healthy People 2023 has 19 objectives targeting heart disease, stroke, and hypertension. Current status of these objectives is showing 10 are baseline, seven are developmental, one has little to no change, and only one as improving. The one objective that is improving is reducing coronary heart disease deaths. In 2018 there were 90.9 coronary heart disease deaths per 100,000 population. Most recent data has shown a decrease to 88.0 coronary heart disease deaths per 100,000 population. The target is 71.0 deaths per 100,000 population.
There are numerous evidence-based programs using novel ways to facilitate improved cardiovascular health. These interventions include increasing daily aspirin use to prevent heart attacks, providing behavioral health therapy to lower CVD risk factors, and self-monitoring blood pressure programs. See the full list here.
The Million Hearts program is a national intervention aimed to prevent 1 million heart attacks and strokes in five years. To accomplish this goal, there are interventions at all levels of the multi-causation model. Click here to learn more about the Million Hearts Program.
recall quiz
Discussion questions
- Describe at least one evidence-based resource for health disease and stroke at this link.
- Refer to the multi-causation model in Chapter 2, and link CV disease to as many of the causes noted on the model as possible. Justify your answers.
Chapter activities
- Read this article, in particular Tables 1 and 2 near the end of the article contrasting the traditional 10 tips for health with the 10 social determinants of health. How do these lists differ? Based on the list of 10 social determinants, how may we need to focus public health efforts to improve population health?
- Use the CDC’s Interactive Map to explore social and environmental data among counties in a state of your choice. At the state level, compare health disease and stroke data among regions in the United States. Describe your findings.
- Complete the stroke risk quiz here. What were your results? We you able to answer all of the questions about your health? If not, what should you do? How could this be used as part of a public health program?
references
American Heart Association. (n.d.-a). Health care professional discussion guide: High blood pressure. Retrieved November 15, 2022, from https://www.heart.org/en/health-topics/high-blood-pressure/commit-to-a-plan-to-lower-your-blood-pressure/doctor-discussion-guide
American Heart Association. (n.d.-b). The facts about high blood pressure. Retrieved November 15, 2022, from https://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure?gclid=Cj0KCQjw39uYBhCLARIsAD_SzMRrS_5Kr9yYprAvxA4gFFF-8f-414Ri5KCEK1rCNs3z_EhFVv20E8waAp8BEALw_wcB
American Heart Association. (2009). What is atrial fibrillation (AFib or AF)? https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af
American Heart Association. (2016a). Bradycardia: Slow heart rate. https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/bradycardia–slow-heart-rate
American Heart Association. (2016b). Prevention and treatment of arrhythmia. https://www.heart.org/en/health-topics/arrhythmia/prevention–treatment-of-arrhythmia
American Heart Association. (2016c). Tachycardia: Fast heart rate. https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/tachycardia–fast-heart-rate
American Heart Association. (2016d). Ventricular fibrillation. https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/ventricular-fibrillation
American Heart Association. (2017, May 31). What is cardiovascular disease? https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease
American Heart Association. (2020). Cardiovascular media library. https://watchlearnlive.heart.org/index.php?moduleSelect=arrhyt
American Heart Association. (2021). Understanding blood pressure readings. https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings
American Heart Association. (2022). Cardiovascular media library. https://watchlearnlive.heart.org/?moduleSelect=tisatk
American Stroke Association. (2018). Stroke symptoms. https://www.stroke.org/en/about-stroke/stroke-symptoms
American Stroke Association. (2019). Effects of stroke. https://www.stroke.org/en/about-stroke/effects-of-stroke
American Stroke Association. (2022). About stroke. https://www.stroke.org/en/about-stroke
Baptiste, D.-L., Turkson-Ocran, R.-A., Han, H.-R., Himmelfarb, C. D., & Commodore-Mensah, Y. (2021). Social determinants of emergency department visits among persons diagnosed with coronary heart disease and stroke. Ethnicity & Disease, 31(1), 41–46. https://doi.org/10.18865/ed.31.1.41
Centers for Disease Control and Prevention. (2019, December 9). Coronary artery disease. https://www.cdc.gov/heartdisease/coronary_ad.htm#:~:text=Coronary%20artery%20disease%20(CAD)%20is
Cleveland Clinic. (n.d.). What to know about essential hypertension (primary hypertension). https://my.clevelandclinic.org/health/diseases/22024-primary-hypertension-formerly-known-as-essential-hypertension
Cleveland Clinic. (2022). Understanding heart failure. https://my.clevelandclinic.org/health/diseases/17069-heart-failure-understanding-heart-failure
Commodore-Mensah, Y., Turkson-Ocran, R.-A., Foti, K., Cooper, L. A., & Himmelfarb, C. D. (2021). Associations between social determinants and hypertension, stage 2 hypertension, and controlled blood pressure among men and women in the United States. American Journal of Hypertension, 34(7), 707–717. https://doi.org/10.1093/ajh/hpab011
Hamann, B. (2007). Disease: Identification, Prevention, and Control (3rd ed.). McGraw-Hill Higher Education.
Havranek, E. P., Mujahid, M. S., Barr, D. A., Blair, I. V., Cohen, M. S., Cruz-Flores, S., Davey-Smith, G., Dennison-Himmelfarb, C. R., Lauer, M. S., Lockwood, D. W., Rosal, M., & Yancy, C. W. (2015). Social determinants of risk and outcomes for cardiovascular disease. Circulation, 132(9), 873–898. https://doi.org/10.1161/cir.0000000000000228
Kreatsoulas, C., & Anand, S. S. (2010). The impact of social determinants on cardiovascular disease. The Canadian Journal of Cardiology, 26 Suppl C(Suppl C), 8C13C. https://doi.org/10.1016/s0828-282x(10)71075-8
Mayo Clinic. (2020, March 6). Caffeine: How much is too much? https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/caffeine/art-20045678
Mayo Clinic. (2022, July 1). Arteriosclerosis: Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569
Niakouei, A., Tehrani, M., & Fulton, L. (2020). Health disparities and cardiovascular disease. Healthcare, 8(1), 65. https://doi.org/10.3390/healthcare8010065
Powell-Wiley, T.M., et al. (2022). Social determinants of cardiovascular disease. Circulation Research, 130, 782–799
Thomas, J. L., & Braus, P. A. (1998). Coronary artery disease in women. Archives of Internal Medicine, 158(4), 333. https://doi.org/10.1001/archinte.158.4.333
U.S. Department of Health and Human Services. (2020). Heart disease and stroke: Healthy People 2023. Health.gov. https://health.gov/healthypeople/objectives-and-data/browse-objectives/heart-disease-and-stroke
Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., Chamberlain, A. M., Chang, A. R., Cheng, S., Delling, F. N., Djousse, L., Elkind, M. S. V., Ferguson, J. F., Fornage, M., Khan, S. S., Kissela, B. M., Knutson, K. L., Kwan, T. W., …Lackland, D. T. (2020). Heart disease and stroke statistics—2020 update. Circulation, 141(9). https://doi.org/10.1161/cir.0000000000000757
(heart + vessels)
brain + vessels

