8 Chapter 8: Sexually Transmitted Infections (STI’s)
Brandye Nobiling

Chapter Objectives
- Differentiate STI’s based on their infectious agent.
- Identify how STI’s are transmitted.
- Identify possible signs and symptoms of bacterial, viral, and parasitic STI’s.
- Identify complications of bacterial, viral, and parasitic STI’s.
- Identify treatment of bacterial, viral, and parasitic STI’s.
- Discuss individuals at elevated risk for STI’s.
- Analyze current trends in reported cases of bacterial and viral STI’s.
- Recognize forms of primary and secondary prevention for STI’s.
Introduction
This chapter covers infections that are commonly transmitted via sexual contact. But, sexual contact is not the only way these infections can be passed. Some can be passed via blood, skin-to-skin contact, from mother to baby in utero or through breast milk, and through sharing contaminated needles. In this chapter you first will explore basic characteristics of each STI – individuals at risk, current rates in the United States, signs/symptoms, transmission, complications, treatment, and prevention. The second section of the chapter covers important prevention and management practices, including proper condom use and how to find local community resources for testing, treatment, management, and prevention. STIs are identified by their infectious agent. There are bacterial, viral, and parasitic STIs.
Bacterial STIs covered in this chapter:
- Chlamydia
- Gonorrhea
- Syphilis
- Primary syphilis
- Secondary syphilis
- Tertiary syphilis
Viral STIs covered in this chapter :
- Human Immunodeficiency Virus (HIV)
- Herpes Simplex 1 and 2 (HSV 1/HSV 2)
- Human Papillomavirus (HPV)
- Genital Warts (low-risk strains)
- High-risk strains
Parasitic STIs covered in this chapter:
- Trichomoniasis
- Pubic lice
Bacterial sti’s
Chlamydia
Overview:
Chlamydia is caused by the bacterium Chlamydia trachomatis, and is the most commonly reported bacterial STI in the United States. Annually, over 1.5 million cases are reported to the CDC from each state health department. In addition, the CDC estimates there is an additional several million cases that go unreported each year. For example, the CDC estimates there were four million cases of chlamydia in 2018. One reason that so many cases go unreported is the asymptomatic nature of the infection. Only 25% of women/people with a vagina and 50% of men/people with a penis who are infected with Chlamydia have signs or symptoms. For this reason, chlamydia is called the “silent STI”.
Individuals at risk:
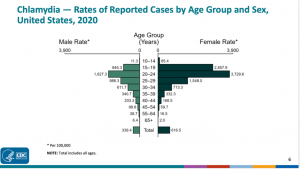
The majority of chlamydia cases are in individuals 15-24 years of age. According to the CDC, in 2020, this age range accounted for 61% of chlamydia cases. It is recommended that women/people with a vagina under 25 years of age and over 25 years of age with risk factors such as having new sexual partners, should get an annual chlamydia screening. Men/people with a penis who have sex with men/people with a penis (MSM) are also at higher risk of contracting STIs. MSM may identify as any type of sexual orientation, including but not limited to: heterosexual, gay, bisexual, pansexual, or demisexual
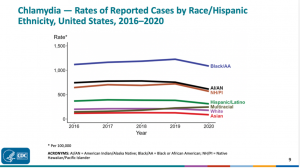
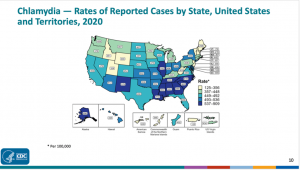
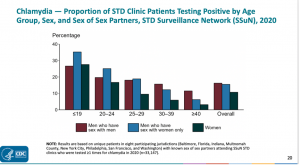
The below charts illustrate chlamydia rates by age, sex (the CDC uses binary male/female), race, ethnicity, geographic region, and reported sexual behavior. From these charts, it is apparent that chlamydia is most reported in:
- Individuals 15-24 years of age
- Women
- Racial and ethnic minorities
- Southeastern states of the US
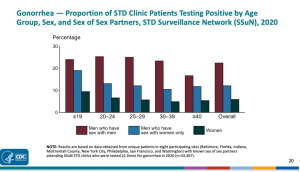
Based on reported sexual behaviors and using binary terms for sex, chlamydia rates are highest among younger men who have sex with women only. At and after the age of 30, however, rates are higher among men who have sex with men.
Transmission:
Chlamydia can be transmitted via oral, vaginal, and anal sex from a person already infected to their partner(s) who are not infected. Ejaculation does not have to occur for chlamydia to be passed. Signs and symptoms, when present, appear based on which route the infection was transmitted. Initial symptoms usually target the throat, genitals, urinary tract, and/or rectum.
The basic formula for STI transmission based on sexual activity:
Oral sex:
- From infected partner’s genitals to their partner’s mouth/throat
- From infected partner’s mouth/through to their partner’s genitals
- From infected partner’s anus to their partner’s mouth
- From infected partner’s mouth to their partner’s anus
Vaginal sex:
- From infected partner’s genitals to their partner’s genitals
Anal sex:
- From infected partner’s anus to their partner’s genitals (typically penis)
- From infected partner’s genitals (typically penis) to their partner’s anus
Chlamydia can also be transmitted from infected mother to their baby during vaginal birth. Chlamydia infection in newborns usually presents as conjunctivitis (i.e. eye infection).
Signs/Symptoms:
When signs and symptoms are present they may include:
- Abnormal vaginal discharge and burning while urinating
- If the infection has spread from cervix to the fallopian tubes, women may experience lower abdominal pain, low back pain, nausea, fever, pain during intercourse, and breakthrough bleeding
- If the infection spreads from cervix to rectum, women may experience to pain, discharge, or bleeding from the rectum
- If transmission occurred during anal sex, they may experience pain or bleeding from rectum
- If transmission occurred during oral sex, they may experience a sore throat
- Discharge from penis or burning while urinating
- Painful and swollen testes
- Burning or itching around penis opening
- If transmission occurred during anal sex, they may experience pain or bleeding from rectum
- If transmission occurred during oral sex, they may experience a sore throat
Complications:
If left untreated, chlamydia can lead to pelvic inflammatory disease (PID). PID can increase risk for ectopic pregnancy, infertility, and scar tissue in the reproductive tract. PID is still a treatable condition with aggressive antibiotic therapy, but any damage already caused by PID cannot be reversed. Click this link to learn more about PID.
Treatment:
Chlamydia is diagnosed via a urine sample or by swabbing the infected area. If detected early, chlamydia can be treated fairly easily with antibiotics. Subsequent infection can happen, and each time someone tests positive for chlamydia, they will have to undergo antibiotic therapy to treat the infection.
Prevention:
Using barrier methods (e.g. latex or polyurethane/polyisoprene condoms and dental/trust dams) during sexual activity is the best primary prevention against chlamydia transmission. If someone tests positive, they should abstain from sexual activity until the infection is treated. More information on STI prevention is found later in the chapter.
Gonorrhea
Overview:
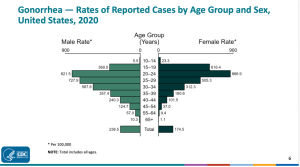
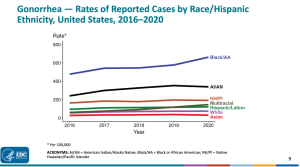
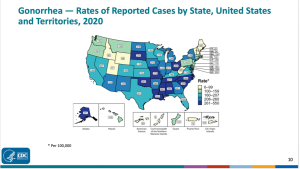
Gonorrhea is caused by the bacterium Neisseria gonorrhoeae, and is the second most commonly reported bacterial STI in the United States. In 2020, over 666,000 cases were reported to the CDC, and the CDC estimates about a million additional cases that go unreported.
Individuals at risk:
Unlike chlamydia, reported male rates of gonorrhea are higher, on average. Gonorrhea rates also are consistently higher among MSM throughout all age groups. Younger women/people with a vagina, between the ages of 15-24 are also at a higher risk for infection. Ethnic and racial minorities have higher reported rates compared to white, non-Hispanic individuals.
Transmission:
Gonorrhea can be transmitted via oral, vaginal, and anal sex from a person already infected to their partner(s) who are not infected. Ejaculation does not have to occur for chlamydia to be passed. Signs and symptoms, when present, appear based on which route the infection was transmitted. Initial symptoms usually target the throat, genitals, urinary tract, and/or rectum.
The basic formula for STI transmission based on sexual activity:
Oral sex:
- From infected partner’s genitals to their partner’s mouth/throat
- From infected partner’s mouth/through to their partner’s genitals
- From infected partner’s anus to their partner’s mouth
- From infected partner’s mouth to their partner’s anus
Vaginal sex:
- From infected partner’s genitals to their partner’s genitals
Anal sex:
- From infected partner’s anus to their partner’s genitals (typically penis)
- From infected partner’s genitals (typically penis) to their partner’s anus
Gonorrhea can also be transmitted from infected mother to their baby during vaginal birth. Gonorrhea infection in newborns usually presents as conjunctivitis (i.e., eye infection).
Because routes of transmission are the same for many STI’s, it is possible for more than one STI to be transmitted from partner to partner, resulting in a diagnosis of more than one type of STI. For example, it is common for someone to be infected with chlamydia and gonorrhea. Proper testing and treatment for each STI is crucial.
Signs/Symptoms:
The signs and symptoms of gonorrhea mirror those of chlamydia, and it is common for infected individuals – especially women – to be asymptomatic.
Signs/symptoms:
When signs and symptoms are present they may include:
- Abnormal vaginal discharge and burning while urinating
- If the infection has spread from cervix to the fallopian tubes, women may experience lower abdominal pain, low back pain, nausea, fever, pain during intercourse, and breakthrough bleeding
- If the infection spreads from cervix to rectum, women may experience to pain, discharge, or bleeding from the rectum
- If transmission occurred during anal sex, they may experience pain or bleeding from rectum
- If transmission occurred during oral sex, they may experience a sore throat
- Discharge from penis or burning while urinating
- Painful and swollen testes
- Burning or itching around penis opening
- If transmission occurred during anal sex, they may experience pain or bleeding from rectum
- If transmission occurred during oral sex, they may experience a sore throat
Complications:
Just like chlamydia, if left untreated, gonorrhea can cause PID, which can increase risk for ectopic pregnancy , infertility, and scar tissue in the reproductive tract. Untreated gonorrhea can lead to scar tissue in the vas deferens which may affect fertility. Untreated gonorrhea may also cause more systemic issues of the blood and joints.
Treatment:
Gonorrhea is diagnosed via a urine sample or by swabbing the infected area Gonorrhea is a bacterial infection, and therefore is treated with antibiotics. One concern about gonorrhea, specifically, is the increasing antibiotic resistance of the bacterium. Watch this video to learn more about this public health issue.
Prevention:
Using barrier methods (e.g., latex or polyurethane/polyisoprene condoms and dental/trust dams) during sexual activity is the best primary prevention against gonorrhea transmission. If someone tests positive, they should abstain from sexual activity until the infection is treated. More information on STI prevention is found later in the chapter.
Syphilis
Overview:
Syphilis is a bacterial infection caused by the bacterium Treponema pallidum. Syphilis affects the body in four progressive stages: Primary, secondary, latent, and tertiary. The infection can be cured with antibiotics in the early stages, but if left untreated will progress to the next stage. Tertiary syphilis cannot be cured and commonly leads to death.
Its existence dates back to Before Common Era (BCE) when Hippocrates described syphilis in 460 BCE. While there is debate on the origin of the infection, the most-supported theory is the one of Columbus and his seamen brought the disease back to Spain after their return from The New World. Columbus ultimately died from syphilis. It is thought that other historical figures also succumbed to syphilis, including Adolph Hitler and Al Capone. Historical research has since shown that Hitler likely did not die of syphilis, but his symptoms of blindness, tremors, skin lesions, paranoia, and possible dementia mimicked neurological complications of the infection in its tertiary stage. In fact, symptoms of tertiary syphilis could be linked to a myriad of various diseases, contributing to the decades of uncertainty over the reason for Hitler’s death. For this reason, syphilis was coined “The Great Imitator” because its tertiary stage signs and symptoms mimic so many other diseases. It has been documented, however, that Al Capone did have syphilis, and it was because of his advanced syphilis diagnosis that he was released from Alcatraz prison in the late 1930’s. Capone eventually died from complications of tertiary syphilis at the age of 48.
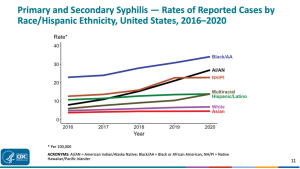
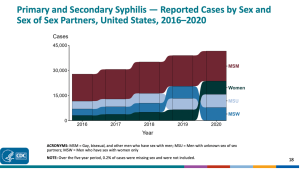
The discovery of penicillin that was discussed in Chapter 1 led to a significant drop in syphilis cases. Since the 1940’s, however, cases in the United States have ebbed and flowed. There have been times where cases have risen and fallen due to compounding factors over the past 80 years. For example, there was a syphilis epidemic that began in 1986 likely due to an increase in drug use, unprotected sex, and lack of access to healthcare among those at highest risk for contracting syphilis. In the early 1990’s, however, rates began to decline and remained relatively low for many years. But, over the past several years, cases are rising again, especially among MSM.
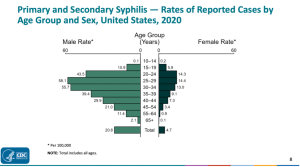
Individuals at Risk:
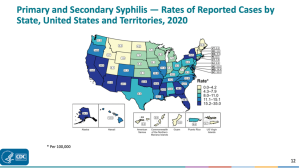
Current rates of syphilis show men who report MSM are the most at-risk of contracting syphilis. According to the CDC, MSM accounted for 43% of primary and secondary syphilis cases in 2020. Rates of syphilis in women/people with a vagina are on the rise, however, which can also increase the risk of congenital syphilis, passed from mother to newborn. Racial and ethnic minorities are also at a disproportionate risk for contracting syphilis compared to white non-Hispanic individuals. Rates are also highest in southwest and southeast regions of the United States and Hawaii. This could be due to several factors, including: 1). Lack of access to healthcare in remote/rural areas, 2). Discrimination of sexual minorities due to biased societal beliefs that prevent MSM from seeking medical care, and 3). Insufficient sexuality education in schools and communities.
Transmission:
Syphilis is passed through all forms of sexual contact. The basic formula for STI transmission based on sexual activity:
Oral sex:
- From infected partner’s genitals to their partner’s mouth/throat
- From infected partner’s mouth/through to their partner’s genitals
- From infected partner’s anus to their partner’s mouth
- From infected partner’s mouth to their partner’s anus
Vaginal sex:
- From infected partner’s genitals to their partner’s genitals
Anal sex:
- From infected partner’s anus to their partner’s genitals (typically penis)
- From infected partner’s genitals (typically penis) to their partner’s anus
Additionally, in the primary stage of syphilis, a lesion called a chancre (pronounced “shane-ker”) usually appears. Direct contact with a chancre can transmit syphilis. In the secondary stage of syphilis, a rash develops on the palms of the hands and bottoms of the feet. Contact with these blisters can transmit syphilis. Congenital syphilis is transmitted from a mother who has syphilis to her newborn.
Signs/Symptoms:
There are four distinct phases of syphilis that are progressive in nature: Primary, secondary, and tertiary. Additionally, there is a latent stage between stages when no signs or symptoms are present. The latent stage occurs after the secondary stage and some individuals will remain in the latent stage, never progressing to the tertiary stage. Here is the breakdown of signs and symptoms for each stage according to The Cleveland Clinic (2022, paras. 3-7):
Primary syphilis: The first stage happens two to 12 weeks after exposure to the bacteria. During this stage, a smooth, red sore called a chancre develops on the genitals or in the mouth. It goes away on its own in a few weeks or months. A chancre is small and usually painless, so you may not even know it’s there.
Secondary syphilis: About one to six months after the chancre goes away, a rough, bumpy syphilis rash appears on the body, usually on your palms and soles (bottoms) of your feet. You may also have flu-like symptoms such as fever, fatigue, sore throat and muscle aches. These symptoms can come and go for months or years.
Latent syphilis: If syphilis isn’t treated during the first two stages, the infection moves into the latent stage. Although there are no outward signs or symptoms of syphilis during this phase, the infection can damage your heart, bones, nerves and organs. This stage can last several years.
Tertiary (late) syphilis: For many people, symptoms don’t progress past the latent phase, either because the infection cures itself or because symptoms are too mild to notice. About a third of people progress to the late syphilis phase, which causes a range of serious health problems. These problems occur slowly and include:
- Brain damage, dementia and mental health problems.
- Heart disease.
- Movement disorders and muscle problems.
- Nerve damage.
- Seizures.
- Tumors, usually on the bones and skin.
- Vision problems.
Complications:
Complications of syphilis are mentioned above under signs and symptoms of tertiary syphilis. These complications ultimately can lead to death.
Treatment:
Syphilis is commonly diagnosed after running a lab sample of blood or cerebrospinal fluid. Syphilis is a bacterial infection treated with antibiotics, specifically penicillin. Primary and secondary syphilis are relatively easy to cure with penicillin if diagnosed early enough. Congenital syphilis is also treated with penicillin. Tertiary syphilis cannot be cured with penicillin.
Prevention:
Using barrier methods (e.g., latex or polyurethane/polyisoprene condoms and dental/trust dams) during sexual activity is the best primary prevention against syphilis transmission. Any contact with a chancre or blisters should be avoided. If someone tests positive, they should abstain from sexual activity until the infection is treated. More information on STI prevention is found later in the chapter.
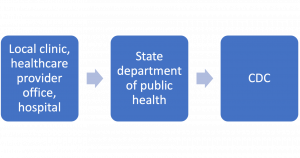
STI’s as Notifiable Diseases
Chlamydia, gonorrhea, and syphilis are all notifiable diseases. A notifiable disease is any condition that requires systematic reporting to the CDC. When someone tests positive for a notifiable disease, that number gets reported at the local clinic, hospital, or healthcare provider office. Those numbers then get reported to the state department of public health. Each state department of public health reports their statistics to the CDC. No names are ever connected to positive cases. Cases are reported as aggregate data. For the current data on all infectious notifiable diseases click here.
Figure 8.3 National Notifiable Diseases Surveillance System (NNDSS):
Viral STI’s
Human Immunodeficiency Virus (HIV)
Overview:
Human Immunodeficiency Virus (HIV) is a viral infection that is spread through bodily fluids: semen, pre-ejaculatory fluid, vaginal secretions, rectal secretions, blood, and breast milk. Once the virus has entered the body it starts to attack CD4 T-cells (also called helper T cells) which are crucial to maintain a healthy immune system.
Watch this video to learn how HIV attacks the immune system.
With new advances in treatment, individuals can live a long and healthy life being HIV-positive. If the virus continues to wear down the body’s defense system, however, an HIV-positive individual may be diagnosed with Acute Immunodeficiency Syndrome (AIDS). In order to be diagnosed with AIDS, a person must have a t-cell count below 200 or an opportunistic infection or disease, such as cancer. Opportunistic infections are infections (viral, bacterial, fungal, parasitic) that disproportionally affect individuals with weakened immune systems due to another infection (e.g., HIV) or disease (e.g. cancer).
The way HIV is treated and managed today is the result of over 40 years of research and development. Click on this link to read the history of HIV/AIDS.
Individuals at Risk:
Anyone who engages in unprotected sex or shares needles is potentially at risk of contracting HIV. Some groups, however, have higher rates of HIV. MSM and racial and ethnic minorities (particularly black/African American and Hispanic individuals) have higher prevalence rates. Also, individuals who have another STI, such as chlamydia and gonorrhea, are also at an elevated risk of contracting HIV.
Click on this link to an interactive webpage and explore HIV rates by year in the United States.
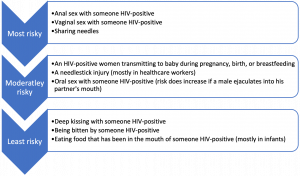
Transmission:
As stated above, HIV is transmitted via the following fluids:
- Semen
- Pre-ejaculatory fluid
- Vaginal secretions
- Rectal secretions
- Blood
- Breast milk
Behaviors that put someone at risk for HIV infection fall under a range of more at risk for contracting HIV to less at risk for HIV. These behaviors are outlined in Figure 8.14
This interactive tool helps you to estimate your risk.
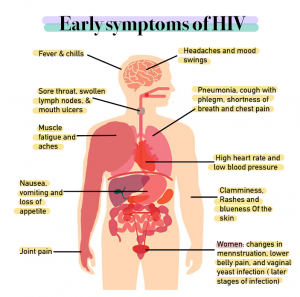
Signs/Symptoms:
Signs and symptoms of HIV vary from person to person, and a number of body systems can be affected. Many people who have been infected with HIV will not experience any symptoms. This underscores the importance of regular testing. If present, some early HIV symptoms are illustrated in Figure 8.15.
Complications:
HIV/AIDS can be broken down into three stages based on signs, symptoms, and complications. There is an acute stage which occurs a few weeks after infection. This stage is followed by a clinical latency stage, also referred to as chronic HIV infection. During this stage, symptoms may be mild (if present at all), but the virus is still multiplying in the body. Proper antiviral treatment in these stages is vital to remain at an HIV-positive diagnosis without progressing into an AIDS diagnosis. If this does not occur the third stage is AIDS. AIDS can cause many complications to organ systems and can lead to death. Click on this link to read more about these stages.
Treatment:
There is no cure for HIV, but with the advances in treatment, HIV-positive individuals can live a long and healthy life. The goal of HIV treatment is to maintain what is called “low viral load” which essentially means that the virus is undetectable. This goal is accomplished through antiretroviral therapy (ART) medication in the form of shots or pills. It is vital for someone who tests positive for HIV get started on therapy as soon as possible, and discuss the right treatment plan with their healthcare provider. Read the information on this link to learn more about how to navigate HIV treatment.
Managing the viral load should not be the only concern when treating HIV. Research has shown that HIV-positive individuals have higher risk for behavioral health issues, such as risky behaviors and some mental health conditions. Interventions at the patient-provider level and community level should focus on these challenges.
Prevention:
Using barrier methods (e.g., latex or polyurethane/polyisoprene condoms and dental/trust dams) during sexual activity is important to prevent the spread of HIV. Needle exchange programs aim to prevent sharing potentially contaminated needles among intravenous drug (IVD) users.
Pre-exposure prophylaxis, better known as PrEP, is antiretroviral medication prescribed to prevent HIV transmission prior to possible exposure. Any licensed healthcare professional can prescribe PrEP. Table 8 outlines the three FDA-approved medications that can be used as PrEP.
Table 8. PrEP Medications
| Medication | Best for |
|
Emtricitabine/tenofovir disoproxil fumarate pills – brand name Truvada® – daily oral medication
|
Preventing HIV infection in those at risk through sex or injection drug use . |
|
Emtricitabine/tenofovir pills– brand name Descovy® – daily oral medication
|
Preventing HIV infection among people at risk through sex, but is not yet approved to protect against HIV transmission in receptive vaginal sex. |
|
Cabotegravir injection (brand name Apretude® – injection given by healthcare provider every two months
|
Preventing HIV infection among all people at risk through sex who may prefer getting an injection every 2 months instead of taking a daily pill or who may not be candidates for a daily pill |
Several studies have shown PrEP to be up to 84% effective at preventing HIV transmission during drug use and 99% effective at preventing HIV during sex. PrEP causes minimal side effects with the exception being among individuals with kidney damage. In those individuals, the injection should be prescribed as it has been shown to have less damage on kidney function. PrEP is a true preventative and should not be taken by someone who has HIV.
Post-exposure prophylaxis, better known as PEP, is an antiretroviral medication prescribed by a healthcare provider after potential exposure to HIV. PEP is considered to be a secondary prevention measure meant to be used in emergency cases only. PEP should be taken within 72 hours after exposure to be effective.
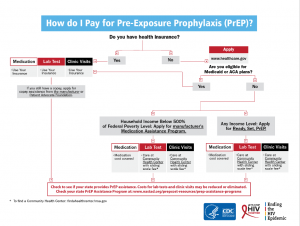
Unfortunately, PrEP and PEP are not typically free. Therefore, someone must have health insurance or can afford to pay out-of-pocket for these preventative services. The CDC created the flowchart in Figure 8.16 to help patients navigate paying for these medications.
Social Determinants of Health and HIV Disparities
HIV cannot be discussed without examining the social determinants of health that impact access to quality healthcare to prevent and treat the infection. Experts have identified HIV as being at the intersection of racism, sexism, poverty, homophobia, and transphobia. Of the 1.5 million people living with HIV in the United States, the majority of them are MSM, transgender women, racial and ethnic minorities, and live in the southern states. Why are these groups disproportionately affected? Social determinants, such as discrimination, lack of access to healthcare, and lack of insurance are to blame. CDC constantly publishes new data on HIV as part of the Medical Monitoring Project in their publication, Morbidity and Mortality Weekly Report (MMWR). In particular, they focus on social determinants of health and how they influence access to care. Read the current report here.
HIV is still considered to be an epidemic in the United States, and, therefore is an infectious disease of public health concern. The Human Resources and Services Administration (HRSA) has established multi-million-dollar legislation to decrease the number of new HIV cases in the United States. The outcome objective for this program is to reduce the number of new HIV infections in the United States by at least 90% by 2030, which would be fewer than 3,000 per year. Click on this link to learn more about this initiative.
Some of the funding for the Ending the HIV Epidemic in the United States initiative is from the Ryan White HIV/AIDS Program. Ryan White was a young virginal teen with hemophilia who contracted HIV from a blood transfusion and died of AIDS in 1990, one month before his high school graduation. Ryan gave a new face to the disease during a time of stigma that presumed HIV/AIDS as a “gay disease”. His story gave the public a new perspective about who can be at risk for the disease. Still going strong 30 years later, the Ryan White HIV/AIDS Program provides resources to people living with HIV and AIDS. Watch this video to learn about this program.
Read more about Ryan’s life here.
World AIDS Day – Uniting and Advocating Against AIDS
December 1st was declared World AIDS Day in 1988 to help raise awareness of the disease and remember the lives lost to the pandemic across the globe. People are encouraged to participate in World AIDS Day in their school, university, workplace, or community. Click here to read what you can do to raise awareness on World AIDS Day.

HIV Criminalization
HIV Criminalization uses laws against people living with HIV merely based on their HIV-positive status. HIV criminalization laws exists in the United States and other countries. These laws can have negative impacts on people living with HIV.
In the United States, 35 states criminalize HIV. Visit here to examine U.S. HIV laws. These laws were created prior to current medical advancement and do not reflect the current state of society. Now, antiretroviral therapy (ART) and pre-exposure prophylaxis (PrEP) allow people to live without fear of transmission or contraction of HIV. HIV criminalization laws go so far as to criminalize behavior that could potentially spread HIV without the actual transmission or intent to transmit. In the United States, black men are disproportionately affected by HIV criminalization laws. Often, it is the case these laws were put in place to discriminate against disadvantaged minority communities such as gay men, sex workers, people of color, and transgender people.
HIV Criminalization is a global issue. One hundred thirty countries criminalize HIV. Explore global HIV laws here. The stigma of HIV, homophobia and transphobia live on strongly in many of these countries. There have been mass arrests of gay men in Egypt, Uganda, and Senegal linked to these fears and as religious punishments for what they view has immoral acts . In Canada, indigenous women are strongly affected through HIV criminalization laws.
The unjust laws and fear of criminalization cause communities living with HIV to avoid social services, access health care (specific reproductive health care and testing), legal services. To change the discrimination of HIV criminalization, these laws need be overturned, modernized and de-prioritized. Nine states have modernized or repealed their laws since 2014. Colombia’s and Kenya’s HIV laws were found to be unconstitutional due to human rights and the rights to privacy violations. Changing HIV criminalization is an effort that requires the interdisciplinary support of public health and legislative system.
Herpes Simplex 1 and 2
Overview:
Herpes Simplex 1 (HSV-1) and Herpes Simplex 2 (HSV-2) are viruses associated with sexual or intimate contact. HSV-1 is associated with oral herpes (also known as “cold sores” or “fever blisters”) and HSV-2 is associated with genital herpes. Approximately 90% of cold sores are caused by HSV-1, and the majority of genital herpes are caused by HSV-2. But it is possible to transmit HSV-1 to the genitals and HSV-2 to the mouth.
Both HSV-1 and HSV-2 are relatively common in the United States. Up to 80% of people living in the United States have HSV-1 and 1 in 6 have HSV-2. Globally, approximately two-thirds (67%) of people have HSV-1 and 13% have HSV-2.
Individuals at Risk:
Anyone can get herpes. The asymptomatic nature of both HSV-1 and HSV-2 makes transmitting the infection to a partner possible even when no signs or symptoms are present. There are some biological and lifestyle factors that may increase the risk for initial transmission as well as recurrence of breakouts. Women report higher rates of herpes. People who are immunocompromised; people taking certain medications that suppressed immunity; people who are HIV-positive; people who share utensils, drinks, food; people who engage in unprotected sex; and people who engage in high-contact sports (e.g., wrestling) are at an elevated risk for contracting HSV-1 and HSV-2. Epidemiological data show that HSV-1 and HSV-2 are more common in Hispanic Americans.
Transmission:
HSV-1 is most commonly transmitted via oral-oral contact with an infected person via kissing or sharing items that come into contact with the mouth (e.g., utensils, lipstick, cigarettes, vapes, pipes, etc.). Less commonly, HSV-1 is transmitted via oral-genital contact with an infected person. HSV-2 is most commonly transmitted via genital-genital or genital-anal contact with an infected person. Transmission is more likely when blisters are present, but both strains can be transmitted when a person is asymptomatic. In rare occasions a mother can transmit HSV-2 to her newborn during delivery.
Signs/Symptoms:
As stated above, HSV-1 and HSV-2 are often asymptomatic. It has been suggested that about 20% of sexually active people living in the United States are what is called seropositive, meaning they test positive for herpes. And many of these nearly 40 million people will never present with blisters or have other symptoms. When they are present, however, the cardinal sign is the presence of a blistery rash. In HSV-1 the blisters are typically on or around the mouth and in HSV-2 the blisters are typically around the genitals and/or anus. These blisters tingle, itch, and burn. Additional symptoms may include fever, swollen lymph nodes, and body aches. These symptoms typically occur during the initial infection as opposed to recurring breakouts. Breakouts usually last 2-4 weeks and eventually the blisters go away without any scarring. Many factors determine the frequency of recurring breakouts, including suppressed immunity, hormonal changes, and stress.
Complications:
One complication of herpes is increased risk for HIV. According to the WHO (2022), people with HSV-2 are three times more likely to contract HIV. This is due to a few factors, including suppress immunity, shared risk behaviors, and the increased transmission risk due to blisters serving as portals of entry for HIV infection.
Severe disease associated with herpes is more common in immunocompromised individuals and can include meningoencephalitis and encephalitis and eye infection. Complications of neonatal herpes (caused when a mother with HSV-2 passes the virus to their newborn during birth) include severe neurological disability.
Treatment:
Although there is no cure, HSV-1 and HSV-2 are relatively easy to manage and treat. “It’s all about suppression” has been the tagline for the medication ValtrexÒ, and this is the focus of herpes. The most common medications prescribed to manage herpes are oral antiviral medications including acyclovir, famciclovir and valacyclovir (the generic ValtrexÒ). Topical ointments can also be prescribed or purchased over the counter and include acyclovir and penciclovir.
Prevention:
HSV-1 can be prevented by not kissing or sharing items used by someone who is positive – especially during a breakout. Oral sex should also be avoided. HSV-2 can be prevented by abstaining from sexual contact during a breakout and using condoms and dams when engaging in oral, genital, and anal sex. One caveat about condom use is that depending on the distribution of the blisters, an external condom (also referred to as a male or outside condom) may not cover all of the sores. An internal condom (also referred to as a female or inside condom) may be more effective because it covers more surface area – especially if the vulva is infected.
Testing for herpes is tricky and there are limits to their efficacy. Anyone showing signs or symptoms should contact their healthcare provider who can then perform a visual inspection of blisters if they are present as well as draw a blood sample to test for seropositivity. Testing is a bit more limited for individuals who are asymptomatic. Individuals who have HSV-2 should be tested for HIV.
Human Papillomavirus (HPV)
Overview:
HPV is the most common STI. The CDC estimates there were about 43 million cases in 2018. There are about 120 subtypes of the virus. Some are associated with genital warts and others are associated with increased risk for cervical and other cancers. The types associated with genital warts are considered “low risk” because they pose a lower risk for developing HPV-related cancer. The types associated with cancer risk are considered “high risk”.
Individuals at Risk:
Age is a significant risk factor for contracting HPV. The highest rates of HPV are among individuals 15-24 years of age. In terms of race and ethnicity, black non-Hispanic and Hispanic individuals have the highest rates of HPV.
Transmission:
HPV is transmitted via oral, genital, or anal sex with an infected person. Close and prolonged skin-to-skin contact with an infected person can also transmit the virus.
Signs/Symptoms:
Most people with HPV are asymptomatic. In low-risk types, genital warts can develop at the site of transmission (e.g., mouth, genitals, anus). These warts are about 1-2mm in diameter and are flesh-colored. These warts can cause burning, itching, and painful sexual intercourse. In high-risk types, symptoms of HPV do not appear.
Complications:
According to the CDC, “In most cases (9 out of 10), HPV goes away on its own within two years without health problems. But when HPV does not go away, it can cause health problems like genital warts and cancer”, (CDC, 2022 para. 5). Cervical cancer is the most common HPV-related cancer followed by oropharyngeal (i.e., mouth and throat) cancer.
Depending on what source you read, HPV accounts for nearly every case of cervical cancer case. HPV also accounts for the majority of anal and oropharyngeal cancer cases. Here are the annual HPV-related cancer cases each year.
Treatment:
There is no cure for HPV. Treatment depends on the type of HPV. Genital warts must be treated by a healthcare provider with each breakout. Treatments include removing the warts via lasers or cryotherapy or dissolved with a medication. Unlike blisters caused by herpes, genital warts do not go away on their own after a breakout. Non-wart types of HPV are managed by regular physical exams and pap tests.
Prevention:
Secondary prevention for HPV-related cervical cancer involves a routine clinical exam where a healthcare provider gathers cells from the cervix and tests them for HPV and any abnormal cellular growth. This can be done as a pap test or a primary HPV test. A primary HPV test checks for the presence of high-risk types of HPV infection. A Pap test checks for abnormal cellular growth that potentially can lead to cervical cancer in women. The American College of Gynecologists and Obstetricians (ACOG) recommends a Pap test for people ages 21-29 every three years. People ages 30-65, have three options: a Pap test alone every three years, an HPV/Pap test every 5 years, or a primary HPV test every 5 years. Testing currently does not exist for men/people with a penis.
Primary prevention for HPV is vaccination and proper condom use. The HPV vaccine, now marketed as a cancer prevention vaccine, is FDA-approved for males and females. The CDC recommends either a 2 or 3 dose schedule starting in their preteen years (as early as 9, but typically between 11-12). Read the detailed dose and schedule here.
The reason for starting the vaccine schedule between 9-12 is to build immunity to the infection prior to exposure. Once an individual starts becoming sexually active, they are potentially exposed to HPV, rendering the vaccination less effective.
Proper use of barrier methods during sexual activity is another primary means of prevention for HPV. External and internal condoms and dams should be used every time one engages in oral, vaginal, or anal sex.
Parasitic STI’s
Trichomoniasis
Overview:
Trichomoniasis (aka “trich”, pronounced “trick”) is a parasitic infection often spread through sexual contact. Trich is the most common curable STI.
Individuals at Risk:
Anyone who is sexually active is at potential risk for getting trick. According to the CDC, there were more than two million cases of trich in 2018. Women/people with a vagina are more likely to get trich, in particular older women/people with a vagina.
Transmission:
Trich is spread through sexual contact. Specifically penile-vaginal or vaginal-vaginal contact. It is not commonly spread through oral or anal sex.
Signs/Symptoms:
Trich is usually asymptomatic. Out of the over two million cases annually, only about 30% of those cases will present with signs and symptoms. Symptoms may include genital itching, pain and burning after peeing and ejaculation, and discharge. The cardinal symptom, if present, in will be a foul-smelling (“fishy” smelling) discharge from the vagina.
Complications:
Pregnant individuals infected with trichomoniasis are the most vulnerable to complications. In these cases, the baby may be born prematurely and have a low birth weight. The mother can also pass the infection to the newborn. In non-pregnant women and in men, untreated trich infections can increase risk for cervical and prostate cancer as well as HIV transmission.
Treatment:
Trich can be treated easily with proper medication which involves either one large dose or multiple smaller doses of an oral antibiotic. All infected partners will also need to be treated. It is highly recommended that all partners abstain from sexual contact (especially penile-vaginal or vaginal-vaginal sexual activity) until treatment is complete and the infection is cured. But, as with other curable STI’s (chlamydia, gonorrhea, and syphilis), subsequent infections may occur if someone is re-exposed by someone infected.
Prevention:
Prevention of trich involves using condoms during sexual activity and proper testing.
Pubic Lice
Overview:
The pubic louse (plural: lice) is a parasite that is commonly spread through sexual contact. Pubic lice are also called pubic “crab” lice due to the parasite’s resemblance to a crab. Pubic lice are small but are visible to the naked eye.
Individuals at Risk:
Anyone who is sexually active can get pubic lice. The presence of pubic hair may increase one’s risk for infection due to the hair serving as a host for the lice. Worldwide, the incidence rate of pubic lice is 2%, and this number has been decreasing over the past 20 years. It has been theorized in scientific research that the societal trend in the United States of pubic hair removal may be partly responsible for the decreasing cases of pubic lice.
Transmission:
Pubic lice are most commonly spread through direct sexual contact. In rare cases, they can also be spread via contact with contaminated bedding or clothing. Humans do not get pubic lice from domestic pets or other animals.
Signs/Symptoms:
The presence of the lice or their eggs is the primary sign of infection. The primary symptom is itching in the infected area. The lice attach to pubic hair and less commonly to other hairy areas of the body, including eyelashes and eyebrows.
Complications:
Pubic lice themselves do not cause disease. The most common complication is a secondary bacterial infection caused by excessive scratching of the infected area.
Treatment:
The most common form of treatment in the United States is through a lotion or shampoo containing pyrethrin and piperonyl butoxide (fancy names for “lice killing” medications). Treatment may be nuanced depending on the location of the lice (genitals vs. eyes). Click this link to read the full treatment regimen.
Prevention:
Pubic lice can be prevented by proper condom use during sexual activity. Avoid sharing bedding, clothing, or towels with others. Removing pubic hair could also help prevent the spread of pubic lice. Secondary prevention involves prompt testing and treatment, and properly washing any contaminated objects (i.e., towels, bedding, clothing).
PREVENTING AND MANAGING STI’s
All of the STI’s discussed in this chapter can be prevented and controlled through the same means. Individuals can protect themselves and their partners by using barrier methods each time they engage in sexual behaviors. The following barrier methods are approved to protect against the transmission of STI’s:
Condoms
Latex and non-latex condoms (made of polyurethane or polyisoprene) are highly effective at preventing the spread of STI’s. External condoms (a.k.a. “male” condoms) and internal condoms (a.k.a. “female” condoms) can be purchased OTC and at various healthcare centers (some healthcare centers provide them free of charge). External condoms are worn on the penis or sex toys and internal condoms can be worn in the vagina or anus. Internal condoms are latex free. DO NOT WEAR MORE THAN ONE CONDOM. Choose between an internal or external condom and use it properly. Click on this link to read how to use an external condom properly and this link to read how to use an internal condom properly.
Condoms made of animal skin (e.g. lambskin) are also available, but these condoms are NOT effective at preventing STI’s. They are porous like human skin, and microscopic infectious agents can enter and exit through these pores.
Dams
A “dental” or “trust” dam is a thin sheath of latex that can be placed over the vulva or anus to protect the spread of STI’s via oral-vaginal or oral-anal sex. They can be purchased OTC and on Amazon as well as healthcare centers. They are typically flavored. If a dam is not available, a condom can be altered to be used as a dam. Click on this link to read how to use dental dams safely.

Cots and Gloves
Finger cots (a.k.a. finger condoms) and latex or non-latex gloves (yes, the same gloves you would use when cleaning or in a science lab) can be used to prevent the spread of STI’s via manual sex (i.e. hand-to-genital or hand-to-anal). They can be purchased OTC and on Amazon. Gloves can be purchased anywhere.

Recall quiz
Discussion questions
- What populations are most at risk for the STI’s covered in this chapter? Include specific populations (i.e. race/ethnicity, sex, age, and geographic location) and STI’s and justify your answers.
- Discuss at least three preventative measures for STI’s.
Chapter activities
- Click on this link and enter your zip code on the toolbar located at the top of the page to find HIV prevention services in your area. What services are and are not provided within 25 miles from your zip code? How about 50 miles from your zip code? How could access affect those seeking HIV prevention and management services?
- Use this interactive data tool https://gis.cdc.gov/grasp/nchhstpatlas/charts.html to explore HIV rates and social determinants of health. Answer the following questions:
-
- What age group had the highest rates of HIV cases in 2020?
- Cases of HIV in 2020 were highest in which three races/ethnicities?
- Cases of HIV in 2020 were highest among what populations based on sexual behavior and drug use?
- Cases of HIV in 2020 were highest in which three states?
references
Adams, D. P. (2021). Foundations of Infectious Disease: A Public Health Perspective. Jones & Bartlett.
American College of Obstetricians and Gynecologists. (2021, January). Chlamydia, gonorrhea, and syphilis. https://www.acog.org/womens-health/faqs/chlamydia-gonorrhea-and-syphilis
American Society for Microbiology. (2019, June 17). Revisiting the great imitator: The origin and history of syphilis. https://asm.org/Articles/2019/June/Revisiting-the-Great-Imitator,-Part-I-The-Origin-a
Anderson, A., & Chaney, E. (2009). Pubic lice (Pthirus pubis): History, biology and treatment vs. knowledge and beliefs of US college students. International Journal of Environmental Research and Public Health, 6(2), 592–600. https://doi.org/10.3390/ijerph6020592
Bernard, E. J., Beyrer, C., & Cameron, E., et al. (2021). Ending unjust HIV criminalization: Leave no‐one behind. Journal of the International AIDS Society, 24(2), 1–3. https://doi.org/10.1002/jia2.25681
Centers for Disease Control and Prevention. (2014, January 23). STD facts: Chlamydia. https://www.cdc.gov/std/chlamydia/stdfact-chlamydia.htm
Centers for Disease Control and Prevention. (2019a). Detailed STD facts: Chlamydia. https://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm
Centers for Disease Control and Prevention. (2019b). Lice: Pubic “crab” lice. https://www.cdc.gov/parasites/lice/pubic/index.html
Centers for Disease Control and Prevention. (2019c). STD facts: Gonorrhea. https://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
Centers for Disease Control and Prevention. (2019d). STD facts: Syphilis (detailed). https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm
Centers for Disease Control and Prevention. (2019e). STD facts: Trichomoniasis. https://www.cdc.gov/std/trichomonas/stdfact-trichomoniasis.htm
Centers for Disease Control and Prevention. (2019f). STD risk and oral sex. https://www.cdc.gov/std/healthcomm/stdfact-stdriskandoralsex.htm
Centers for Disease Control and Prevention. (2019g, December 2). Human Papillomavirus (HPV) vaccine. https://www.cdc.gov/hpv/parents/vaccine-for-hpv.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fhpv%2Fvaccine.html
Centers for Disease Control and Prevention. (2020, May 19). Learn about PrEP. https://www.cdc.gov/hiv/clinicians/prevention/prep.html
Centers for Disease Control and Prevention. (2021a, July 22). STI treatment guidelines. https://www.cdc.gov/std/treatment-guidelines/default.htm
Centers for Disease Control and Prevention. (2021b, September 29). National Notifiable Diseases Surveillance System (NNDSS). https://www.cdc.gov/nndss/index.html
Centers for Disease Control and Prevention. (2022a, April 11). Sexually Transmitted Disease surveillance: National overview. https://www.cdc.gov/std/statistics/2020/overview.htm#National
Centers for Disease Control and Prevention. (2022b, April 29). Figures. https://www.cdc.gov/std/statistics/2020/figures.htm
Centers for Disease Control and Prevention. (2022c, July 11). Genital herpes screening. https://www.cdc.gov/std/herpes/screening.htm#:~:text=A%20healthcare%20provider%20may%20diagnose
Dholakia, S., Buckler, J., Jeans, J. P., & et al. (2014). Pubic lice: An endangered species? Sexually Transmitted Diseases, 41(6), 388–391. https://doi.org/10.1097/OLQ.0000000000000142
Greenberg, J., Bruess, C., & Conklin, S. (2010). Exploring the Dimensions of Human Sexuality. Jones & Bartlett Learning.
Hamann, B. (2007). Disease: Identification, Prevention, and Control (3rd ed.). McGraw-Hill Higher Education.
Kreisel, K. M., Spicknall, I. H., Gargano, J. W., & et al. (2021). Sexually transmitted infections among US women and men. Sexually Transmitted Diseases, Publish Ahead of Print(4). https://doi.org/10.1097/olq.0000000000001355
Kreisel, K., Weston, E., Braxton, J., & et al. (2017). Keeping an eye on chlamydia and gonorrhea conjunctivitis in infants in the United States, 2010–2015. Sexually Transmitted Diseases, 44(6), 356–358. https://doi.org/10.1097/olq.0000000000000613
Mayo Clinic. (n.d.-a). HIV/AIDS: Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/hiv-aids/symptoms-causes/syc-20373524#:~:text=You%20can%20have%20an%20HIV
Mayo Clinic. (n.d.-b). Syphilis: Diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/syphilis/diagnosis-treatment/drc-20351762#:~:text=Syphilis%20can%20be%20diagnosed%20by
Mayo Clinic. (2018a). Chlamydia trachomatis: Diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/chlamydia/diagnosis-treatment/drc-20355355
Mayo Clinic. (2018b). Yeast infection in men: How can I tell if I have one? https://www.mayoclinic.org/male-yeast-infection/expert-answers/faq-20058464
NIH’s Office of AIDS Research. (n.d.). Post-exposure prophylaxis (PEP). Retrieved October 25, 2022, from https://hivinfo.nih.gov/understanding-hiv/fact-sheets/post-exposure-prophylaxis-pep#:~:text=PEP%20stands%20for%20post%2Dexposure
Nobiling, B.D. (2015). Use this, not THAT contraceptive! Journal of Health Education Teaching Techniques, 2(1), 47-66.
PBS. (2017, January 25). The infectious disease that sprung Al Capone from Alcatraz. https://www.pbs.org/newshour/health/infectious-disease-sprung-al-capone-alcatraz
Peterman, T. A., Tian, L. H., Metcalf, C. A., & et al. (2006). High incidence of new sexually transmitted infections in the year following a sexually transmitted infection: A case for rescreening. Annals of Internal Medicine, 145(8), 564. https://doi.org/10.7326/0003-4819-145-8-200610170-00005
Sanderson, A., Ranville, F., & Gurney, L., et al. (2021). Indigenous women voicing experiences of HIV stigma and criminalization through art. International Journal of Indigenous Health, 16(2), 267–290. https://doi.org/10.32799/ijih.v16i2.33903
U.S. Department of Health & Human Services. (2018, September 25). Symptoms of HIV. https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/symptoms-of-hiv
Wald, A., Zeh, J., Selke, S., & et al. (2000). Reactivation of Genital Herpes Simplex Virus Type 2 infection in asymptomatic seropositive persons. New England Journal of Medicine, 342(12), 844–850. https://doi.org/10.1056/nejm200003233421203
World Health Organization. (n.d.). Herpes simplex virus. https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus#:~:text=The%20herpes%20simplex%20virus%20(HSV
A sexual orientation in which a person is romantically or sexually attracted to a person of the opposite sex.
A sexual orientation in which someone is romantically or sexually attracted to a person of the same gender.
Someone who is "emotionally, romantically or sexually attracted to more than one sex, gender or gender identity though not necessarily simultaneously, in the same way or to the same degree. Sometimes used interchangeably with pansexual", (HRC, n.d. para 5).
"Someone who has the potential for emotional, romantic or sexual attraction to people of any gender though not necessarily simultaneously, in the same way or to the same degree. Sometimes used interchangeably with bisexual" (HRC, n.d. para 23).
A sexual orientation in which a person develops a sexual attraction to someone only after forming a close bond with them.
Bleeding or spotting in-between periods.
When the fertilized egg implants outside the uterus; typically in the fallopian tube or outside the reproductive anatomy in abdominal cavity.