5 Chapter 5: Fungal Infections
Brandye Nobiling

Chapter Objectives
- Identify fungal infections by the route of transmission.
- Identify individuals most at risk for selected fungal infections.
- Differentiate among the selected types of fungal infections.
- Describe primary and secondary means of prevention for selected fungal infections.
- Recognize the consequences of douching.
INTRODUCTION
Fungi, like bacteria, are living organisms that naturally exist in our environment. Also like bacteria, most fungi are harmless to our health, and in some cases, such as in the gastrointestinal system and vagina, they are helpful to maintain homeostasis. This chapter focuses on fungal infections that can be transmitted through exposure to a fungus in the environment or when there is an overgrowth of a fungus in or on the body.
Histoplasmosis
Histoplasmosis is a fungal infection caused by the fungus Histoplasma capsulatum. It is not transmitted human to human, but rather through contact with soil contaminated with a large amount of bird or bat droppings.
Individuals at risk – People most at risk are those who regularly are in contact with bird and bat droppings. Anyone who works with birds or bats, such as chicken farmers, are more at risk due to their regular exposure to droppings. People with compromised immunity are also at risk for experiencing symptoms of histoplasmosis. Dogs and cats can also get histoplasmosis. Birds cannot get histoplasmosis because their high body temperatures do not create a welcoming environment for the fungus to thrive. Bats, pets, and humans, however, have lower body temperatures and therefore can acquire the infection. Histoplasmosis is more common in the central and eastern states of the US and in certain areas throughout the world, such as Canada and the Caribbean.
Sign/Symptoms – Most cases of histoplasmosis are asymptomatic. If symptoms do appear, however, they include common cold or flu-like symptoms, such as fever chills, headache, cough, body aches, and fatigue.
Transmission –The fungus grows in soil when there is a large amount of bird or bat droppings. Transmission occurs when the spores produced by the fungus are inhaled.
Treatment – Most cases of histoplasmosis do not require medical treatment. In more severe cases, however, anti-fungal medication will be prescribed. The length of the medication regimen depends on the symptoms and severity of the infection.
Complications – Most cases of histoplasmosis go away within a few weeks. Complications can arise in those who are immunocompromised and include serious damage to the lungs, brain, and spinal cord.
Prevention – Preventing contact with contaminated spores can be difficult, but there are ways to intervene in high-risk settings to help reduce exposure. According to the Canadian Centre for Occupational Health and Safety, “prevention of histoplasmosis relies on avoiding exposure to dust in a contaminated environment. Before anyone cleans chicken coops or other contaminated soil, spraying with water is advisable to reduce dust.
Persons working in contaminated areas should use protective clothing such as gloves and coveralls. They should also use a respirator equipped with a high efficiency particulate air (HEPA) filter that is capable of filtering particles down to two microns in size. For major clean up operations of prolonged exposure, a powered air purifying or supplied air respirator may be necessary” (2018, https://www.ccohs.ca/oshanswers/diseases/histopla.html).
tinea
Tinea infections are caused by a fungus that can live and grow on the skin, mucous membranes, hair, nails, feathers, and other body surfaces. Infections are classified according to the body part infected by the fungus:
- Tinea capatis – infection of the scalp
- Tinea cruris – infection of the groin (also called “jock itch”)
- Tinea pedis – infection of the foot/toes (also called “athlete’s foot”)
- Tinea corporis – infection anywhere on the body other than parts that have their own classification, but is most commonly found in the folds of the skin
- Tinea unguium or onychomycosis – infection of the fingernails or toenails
Any tinea infection is generically referred to as “ringworm” as the infection often causes round scaly patches to appear on the skin. Figures 5.1 through 5.5 illustrate the various tinea rashes.





Individuals at risk – Anyone can get a tinea infection, but there are certain factors that can increase one’s risk. Tinea capaits is more common in children than adults. All forms are more common in people who: live in warm climates, have poor hygiene, have compromised immune systems, use communal bathrooms or locker rooms, share towels or other personal hygiene products, and play contact sports.
Signs/Symptoms – In cases of tinea capatis, corporis, and cruris a red, scaly rash will appear on the infected part of the body Tinea pedis causes the skin between the toes to become white, scaly, and blistery. Tinea unguium causes a yellowing and hardening of the nails. Symptoms of all types include itching, burning, and pain.
Transmission – Tinea is very contagious and can spread easily from person to person or pet to person through direct contact. An infected person can also infect themselves from one part of the body to the other. For example, ringworm on the skin (tinea corporis) can spread to the scalp (tinea capatis).
Treatment – Anti-fungal medication is prescribed to treat cases of tinea infection. In addition, keeping the infected area clean and dry will help prevent spreading to other parts of the body.
Complications – In some cases, a kerion will form. A kerion is a large, painful sore that forms over the area of infection caused by hypersensitivity to the tinea fungus. This is treated separately with a steroid medication to reduce inflammation. Other complications caused by tinea infections include swollen lymph nodes and subsequent bacterial infections.
Prevention – Tinea infections can be prevented by practicing good hygiene and not sharing personal hygiene items. Shower shoes should be worn in communal bathrooms and locker rooms. Education programs targeting people who use these types of facilities (e.g. athletes, college students living in residence halls with a shared bathroom) should be a priority. Educating pet parents is also important because infection can be passed from pet-person. Pet parents need to know the signs of ringworm in order to get their furry loved one tested and treated if needed.
The CDC is warning the public about the detrimental effects of using steroid creams on tinea infections. Sometimes the symptoms of tinea infection can mimic other skin issues, such as psoriasis, eczema, or contact dermatitis – all of these are treated with corticosteroid ointments or creams. It’s likely that a person develops ringworm, doesn’t know what it is, and tries their steroid cream on it. After all, it looks like a skin condition they’ve had. This is why it is always important to seek medical diagnosis to properly treat any condition. Studies have shown use of steroid creams on ringworm can cause the infection to further spread and can cause long-term skin problems. Click this link to see photographs and read more about the global impact of steroid cream use for ringworm.
Candidiasis
Candidiasis is a group of fungal infections caused by a type of yeast, called candida. There are a couple of noteworthy strains of candida. Candida albicans is a commonly occurring fungus that lives on the skin, mouth, throat, colon, and vagina as a healthy fungus. In these areas, a flora of healthy bacteria and fungi exist. Maintaining balance of this flora is vital, and when conditions arise that decrease or increase either the bacteria or fungi, infection can result. For example, candida is a healthy fungus that is part of the vaginal flora. If something, such as taking antibiotics or douching, causes a decrease in the healthy bacterial count of the vaginal, there will be an increase in the yeast count, resulting in a vaginal yeast infection.
Individuals at risk – Risk depends on the location of candida infection. Oral candidiasis (also called thrush) is significantly higher in babies. Babies are more at risk because their healthy flora in their mouth has not fully developed. Thrush can also result from antibiotic use by mother or baby. Thrush can also be passed during breastfeeding. The yeast can also be present as diaper rash. In adults, risk for thrush increases in those who wear dentures, smoke, have compromised immune systems, have dry mouth, take antibiotics, have been diagnosed with certain kinds of cancer, and have diabetes. Risk for vaginal candidiasis (also referred to as a yeast infection) include douching, wearing tight pants or underwear made of certain synthetic fabrics, taking antibiotics, pregnancy, having diabetes, and having a compromised immune system.
Signs/Symptoms – The cardinal symptom of thrush is the presence of a white, patchy “cottage cheese” like rash on the tongue and in the back of the throat. Individuals can also experience a sore throat, a cotton-like feeling in the mouth, loss of taste, pain while eating, and cracked lips. Vaginal yeast infections cause a white, odor-free discharge from the vagina as well as burning, itching, swelling, and soreness in the vaginal area. Pain during intercourse is also common with vaginal yeast infections.

Transmission – Because candida albicans naturally exists in the body, infection arises when the natural flora gets disrupted by one or more of the risk factors mentioned above under “individuals at risk”. While vaginal yeast infections are not technically considered a sexually transmitted infection (STI), candidiasis can be passed between partners during vaginal, oral, or anal intercourse.
Treatment – Thrush and vaginal yeast infections are treated with anti-fungal medication that is either applied to the infected area as a cream or ointment, or an oral medication. In more severe cases, longer or more aggressive anti-fungal therapy may be needed.
Complications – Complications from most oral and vaginal yeast infections are rare. In some cases, a woman may have chronic yeast infection and may be prescribed aggressive treatment. The most concerning type of yeast infection emerging in public health is candida auris, and is discussed in Spotlight XX
Prevention – Risk for thrush and vaginal yeast infections can be lowered by practicing good hygiene and avoiding controllable risk factors (e.g., not douching). Both infections can be prevented by a health care provider prescribing an anti-fungal medication (e.g., fluconazole/brand name Diflucan) prophylactically when prescribing an antibiotic. If it’s suspected to have been passed via sexual intercourse, partner(s) at risk should see a health care provider.
Douching is a Douch!
Douching is not recommended because the vagina is a self-cleaning organ. Douching can increase risk for infections such as candidiasis and bacterial vaginosis because it disrupts the healthy flora balance in the vagina. Douching is marketed to women who have that “not so fresh feeling” or who are concerned about vaginal odor. Some foods such as garlic can cause a slight change in vaginal odor or taste, but is reversible by avoiding that food. If a woman has concerns about vaginal odor, she should seek medical consult to rule out the possibility of infection.
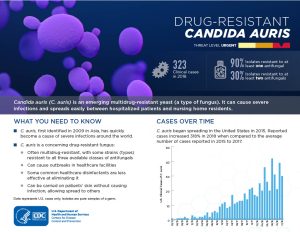
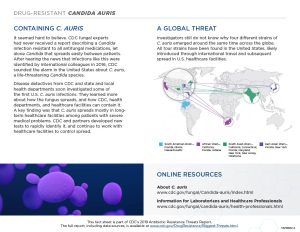
An emerging public health threat is a strain of candidiasis that is resistant to anti-fungal therapy.
recall quiz
discussion questions
- How can histoplasmosis be prevented?
- How can various forms of tinea be prevented?
- A friend mentions she wants to start douching. How would you advise her?
references
Cedars Sinai. (n.d.). Tinea infection. https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/tinea-infection.html
Centers for Disease Control and Prevention. (2019a). Candida auris. https://www.cdc.gov/fungal/candida-auris/index.html
Centers for Disease Control and Prevention. (2019b). Candida infections of the mouth, throat, and esophagus. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html
Centers for Disease Control and Prevention. (2019c). Symptoms of histoplasmosis. https://www.cdc.gov/fungal/diseases/histoplasmosis/symptoms.html
Centers for Disease Control and Prevention. (2019d, January 28). Treatment for histoplasmosis. https://www.cdc.gov/fungal/diseases/histoplasmosis/treatment.html
Centers for Disease Control and Prevention. (2019e, January 29). People at risk for histoplasmosis. https://www.cdc.gov/fungal/diseases/histoplasmosis/risk-prevention.html
Centers for Disease Control and Prevention. (2020, May 14). Steroid creams can make ringworm worse. https://www.cdc.gov/fungal/diseases/ringworm/steroids.html
Centers for Disease Control and Prevention. (2022, September 14). Information for healthcare professionals. https://www.cdc.gov/fungal/diseases/ringworm/health-professionals.html#:~:text=Sources
Ely, J. W., Rosenfeld, S., & Mary Seabury Stone. (2014). Diagnosis and management of tinea infections. American Family Physician, 90(10), 702–710. https://www.aafp.org/afp/2014/1115/p702.html
Government of Canada, C. C. for O. H. and S. (2022, October 6). Histoplasmosis: OSH answers. https://www.ccohs.ca/oshanswers/diseases/histopla.html
Hamann, B. (2007). Disease: Identification, Prevention, and Control (3rd ed.). McGraw-Hill Higher Education.
Icahn School of Medicine at Mount Sinai. (n.d.). Thrush in newborns Information. Mount Sinai Health System. Retrieved October 6, 2022, from https://www.mountsinai.org/health-library/diseases-conditions/thrush-in-newborns#:~:text=Thrush%20often%20occurs%20when%20mother
Mayo Clinic Staff. (2019). Yeast infection (vaginal): Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999
Minnesota Department of Health. (n.d.). Histoplasmosis (Histoplasma capsulatum). https://www.health.state.mn.us/diseases/histoplasmosis/index.html
The Office on Women’s Health. (2018, May 23). Vaginal yeast infections. https://www.womenshealth.gov/a-z-topics/vaginal-yeast-infections
A physiological balance in the body.
“Microorganisms that normally reside at a given site and under normal circumstances do not cause disease.” https://medical-dictionary.thefreedictionary.com/normal+flora